Woman-face-lifted-to-sun.jpg

Photo by dolgachov / 123rf.com
1 Introduction
I am a great fan of sunlight exposure, to both the skin and the eyes. We have been brainwashed into believing that the sun is toxic, whereas in fact it is life-giving. People who live in places with little sun have statistically higher risk to many chronic conditions, such as multiple sclerosis, diabetes, cardiovascular disease, autism, Alzheimer’s disease, and age-related macular degeneration.1 There is a great deal of epidemiological evidence suggesting that sunlight exposure protects from many different types of cancer. The sun has always been a resource for planet earth, and, just as sunlight is essential for plants to grow, I believe it plays an essential role in energizing animals, including humans.
Chances are, you have been told by your dermatologist to “stay out of the sun and take a vitamin D supplement every day.” This seems like good advice, because we have been well trained to believe that the sun causes skin cancer, and the only reason to get out in the sunlight is to boost vitamin D levels through its UV-stimulated synthesis in the skin. Mothers are now well trained to slather sunscreen on their children every few hours on a day at the beach, and they believe that this will keep them safe from skin cancer and has no down side.
The story is not that simple, however. In a paper published in 2016, Richard Weller wrote: “A substantial body of evidence shows that sunlight has health benefits and that these are independent of vitamin D and thus cannot be reproduced by oral supplementation.”2 Since the beginning of time on earth, the sun has always been there. Biological organisms evolved with a constant supply of energy they could count on every day with the rising sun. It is well known that plants use the energy of sunlight to convert inorganic carbon into organic matter, with the help of chlorophyll. Why would animals ignore such an obvious energy source? I believe that animals too have developed a mechanism to safely exploit the sun’s energy – through the oxidation of sulfur to sulfate, and with the help of cholesterol. This reaction takes place in the skin, catalyzed by sunlight, and it is vital to our long-term health.
UV radiation is recommended to treat many different skin conditions, including psoriasis, eczema, jaundice and acne. Sunlight may also be beneficial in various autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus, inflammatorybowel disease, and thyroiditis. Many believe that the benefits of sunlight exposure are mainly due to vitamin D synthesis, and a natural conclusion is that vitamin D supplements would achieve the same goal. However, when placebo-controlled studies are conducted on vitamin D supplementation, they usually produce disappointing results. I believe the reason is that sunlight exposure is about a whole lot more than vitamin D synthesis in the skin.
Those who are familiar with my research will know that I believe that keratinocytes in the skin, endothelial cells lining the walls of surface veins, and red blood cells are able to exploit the energy in sunlight by oxidizing hydrogen sulfide to make sulfate.3 In the skin, the sulfate is conjugated with both vitamin D and cholesterol, and this makes these otherwise water-insoluble molecules water soluble. This greatly faciliates their transport in the blood, because they no longer have to be enclosed inside lipid particles like high-density lipoprotein (HDL) and low-density lipoprotein (LDL). Sunlight exposure thus produces cholesterol sulfate as well as vitamin D sulfate, and it is the cholesterol sulfate that offers many of the benefits that are seen epidemiologically in sunny places. In fact, I believe that systemic sulfate deficiency is a key driver behind many chronic diseases that are on the rise in the industrialized nations.
The sulfate that is produced in response to sunlight also supplies sulfate to the glycocalyx, the mesh of extracellular matrix glycoproteins that line the walls of all blood vessels. Red blood cells hand off cholesterol sulfate to the endothelial cells as they traverse the capillaries, and both the cholesterol and the sulfate are of vital importance to the endothelial cell’s health. The endothelial cells as well can incorporate the sulfate they synthesize themselves, directly into the glycocalyx.
Sulfate in the glycocalyx helps to maintain the structured water in the exclusion zone, a layer of gelled water that coats the surface of all the blood vessels. Not only does the gel provide protection of the wall from oxidative and glycation damage, but it also provides a slick surface for frictionless traversal of the capillary by the red blood cells. And, perhaps most importantly, it carries a negative charge, creating a battery that is likely the main source of electricity for the body. Light, but, most especially, infrared light, causes the exclusion zone water layer to expand dramatically, by as much as a factor of four.4 The electricity held in the battery grows in direct correspondence. Prof. Gerald Pollack from the University of Washington in Seattle has popularized much of this story in his book, Cells, Gels and the Engines of Life.
2 Sunscreen and Melanin
Most Americans heavily rely on sunscreen for sun protection if they are planning to be outside for an extended period. They strongly believe that they are protecting themselves from skin cancer through this practice, but, in fact, they may be increasing their risk to skin cancer. In fact, sunscreen interferes with the body’s natural mechanisms of sun protection, which have been perfected over hundreds of millions of years of life’s evolution on earth.
2.1 Melanoma and Sunscreen
Given how much advertising we get urging us to use sunscreen, people probably assume that there is plenty of evidence that sunscreen protects from skin cancer. If this is true, then it is hard to explain why melanoma prevalence has been steadily rising in step with the rise in the use of higher and higher sun-protection-factor (SPF) sunscreens over the past two decades.
A study published in 2009 analyzed almost 300 million person-years of data over a 10 year period and concluded that the rate of skin melanoma increased by 3.1% per year from 1992 to 2004 in the United States.5 A population-based study published in 2019 involved 12,462 cases of head and neck melanoma in the United States and Canada spanning the interval from 1995 to 2014.6 They found that this type of cancer had increased by 51% over two decades, with males aged 15 to 39 years being the population group most strongly affected. Meanwhile, the sun protection market value increased from 940 million dollars in 2006 to 1.6 billion dollars in 2016.
As far back as 1996, a paper was published that investigated the question of whether sunscreen protects from skin cancer. They wrote: “Our results support the hypothesis that sunscreens do not protect against melanoma, probably because of their ability to delay or avoid sunburn episodes, which may allow prolonged exposure to unfiltered ultraviolet radiation.”7 In other words, sunscreen gives you the illusion that you are safe because you don’t feel the pain or experience the redness of the skin that naturally happens when your body is letting you know it’s time to get out of the sun. Your skin is getting damaged by too much UV radiation, but the signal that would stop the exposure is missing.
Worse than this, in my opinion, is that sunscreen disrupts the body’s natural mechanism of sun protection: melanin synthesis. Sunscreen protection only lasts while the sunscreen is topically present. Melanin, produced in response to sunlight exposure, on the other hand, builds up over time and eventually produces a healthy tan with protection that can last for weeks or even months later. The smart way to protect from the potential damage of UV rays is to develop a tan slowly during the spring while the sun is not so intense, and this arms you with a defense against the intense summer sun that would otherwise be dangerous. The powerful antioxidant effects of melanin protect you from the UV rays, while you can still enjoy the many health benefits of visible light and infrared light, far beyond what you would get from a vitamin D supplement.
Sunscreen also contains toxic ingredients that cause damage to the skin in ways that might result in sustained disruption of sulfate synthesis. Particularly disturbing is the aluminum that is added to emulsify the zinc oxide and titanium dioxide additives (the active ingredients). Aluminum is known to suppress cytochrome P450 enzymes (CYP enzymes), and the enzyme that I propose is crucial for sulfate synthesis, endothelial nitric oxide synthase (eNOS), is an orphan CYP enzyme. I believe that glyphosate, the active ingredient in the pervasive herbicide, Roundup, also disrupts eNOS, since it is known to suppress CYP enzymes in the liver in rat studies. Worse than this, it interferes with the shikimate pathway in the gut microbes, which is essential for producing the aromatic amino acids.8 One of these, tyrosine, is a precursor to melanin, so glyphosate likely induces melanin deficiency, which prevents you from developing a healthy tan, and therefore interferes with natural protective mechanisms against UV damage.
2.2 Melanoma, Sun Exposure and Vitamin D
Instinctively, most people who are diagnosed with skin melanoma make special efforts to avoid the sun following diagnosis, which is probably a very bad idea. Remarkably, increased sun exposure, more frequent sunburns and solar elastosis (evidence of photo-aging in the skin) were all associated with improved survival statistics in a population study on 528 patients diagnosed with cutaneous melanoma.9 It has seemed logical that the reason for the benefit is the rise in vitamin D levels induced by sun exposure.
Indeed, vitamin D deficiency at the time of diagnosis is associated with a worse prognosis in melanoma.10 Patients with stage IV melanoma had a 2-fold worse prognosis if they suffered from vitamin D deficiency at diagnosis. Furthermore those who began with vitamin D deficiency and whose vitamin D levels either fell or increased by no more than 20 ng/mL had a hazard ratio of 4.68 compared to patients who were not deficient initially and whose vitamin D increased by more than 20 ng/mL over time.
However, a large population placdebo-controlled study involving 36,282 postmenopausal women compared women who were supplemented with 400 IU vitamin D3 and 1,000 mg elemental calcium every day for 7 years with controls given a placebo.11 Rates of skin melanoma and non-melanoma skin cancer were monitored over the 7-year period. There was no difference in rates of either benign or malignant cancers between the two groups. This strongly suggests that vitamin D is not the reason for the improved survival with sun exposure.
2.3 Melanin, Infrared Light and Skin Cancer
Melanin is able to transform 99.9% of absorbed sunlight into heat, and this greatly reduces the risk to skin cancer. It also enhances the amount of infrared you can receive from the sun. A fascinating study published in 2017 experimented with a novel idea to protect mice from skin cancer.12 It involved a new technique to treat melanoma skin cancer using a transdermal skin patch, infrared light, and melanin. Melanoma tumor cells produce high amounts of melanin. The researchers created a skin patch from ruptured melanoma cells, which they applied to the skin of mice (as a source of melanin). They compared three groups of mice, the controls, mice with only the patch, and mice with the patch plus infrared light exposure. Viable melanoma cells were subsequently injected into all three groups to induce skin cancer, and 100% of the control group succumbed to melanoma cancer within a two-month period. Among the ones with only the patch, only 13% of the mice survived. Remarkably, those who received both the infrared light and the patch were all still living after two months, and 87% had no tumors. One wonders what would have happened with only infrared and no patch!
3 Sunlight, Vitamin D Supplements and Disease
In this section, I will address evidence that sunlight is protective against four distinct diseases and conditions: cancer, heart disease, hypertension, and bone fractures. In each case, studies have shown that vitamin D supplements cannot replace these benefits of sunlight.
3.1 Cancer
As far back as 1980, epidemiological studies showed an inverse geographical relationship between the amount of solar radiation and mortality rates for colon cancer.13 Since then, numerous studies have shown that a high serum level of vitamin D is associated with reduced cancer risk, for diverse types of cancer. A review paper published in 2018 with 140 references revealed that those with higher serum vitamin D have an improved odds ratio for developing brain cancer, cervical cancer, endometrial cancer, esophageal cancer, gastric adenocarcinoma, head and neck cancer, hepatocellular carcinoma lymphoma, ovarian cancer, and thyroid cancer.14 Furthermore, for many types of cancer, those with higher serum vitamin D at the time of cancer diagnosis have statistically improved survival times.
Given all of this evidence for an association between serum vitamin D levels and cancer protection, it seems obvious that vitamin D supplementation should be protective against cancer. However, a large placebo-controlled study, published in 2019, involving more than fifteen authors, obtained disappointing results.15 In this study, over 25,000 participants were monitored over a five-year period. The study population was restricted to men over 50 years old and women over 55 years old, and all participants lived in various places across the United States. Those who received vitamin D were supplemented with 2000 IU per day. Supplementation did not lower the incidence of invasive cancer or of cardiovascular events, compared to placebo.
3.2 Cardiovascular Disease
Researchers have long been aware that there is a direct relationship, epidemiologically, between cardiovascular disease and latitude. People who live at high latitudes have significantly higher rates of heart disease than those nearer the equator.16 Furthermore, more people suffer from heart attacks in the winter than in the summer, in both northern and southern latitudes.17
We saw above that a large placebo-controlled study did not find any benefit in vitamin D supplementation for heart disease risk. A study based in India is one of very few controlled studies where vitamin D supplementation was compared to sunlight exposure. The study involved 100 men who had been diagnosed with severe vitamin D deficiency.18 Half of them were prescribed supplemental vitamin D (1000 IU/day), and the other half were advised to spend at least 20 minutes out in the sunlight every day during the midday. Both groups saw an increase in their serum vitamin D levels, but, remarkably, the two approaches had opposite effects on serum cholesterol. Those exposed to sunlight saw a statistically significant drop in their total cholesterol, and those with the supplement saw a statistically significant increase.
This makes sense to me, because vitamin D supplements are fat soluble, and they require the liver to synthesize cholesterol and release LDL particles in order to transport the vitamin D. Sunlight exposure stimulates cholesterol sulfate synthesis in the skin, and the sulfate moiety makes the molecule water soluble.3 This means that it can be transported in the blood without being packaged up inside an LDL particle. Because it is both water soluble and fat soluble, cholesterol sulfate can easily traverse water-based media to be transferred from the membrane of a cell in the skin to the membrane of an HDL particle or a red blood cell, and it can also easily be transferred to a tissue cell in need of additional cholesterol. Hence, sulfation, induced by sunlight, promotes efficient delivery of cholesterol to the tissues, without the need for LDL carrier particles. These ideas are schematized in Figure 1.
Differences-between-sunlight-exposure-and-vitaminD.jpg
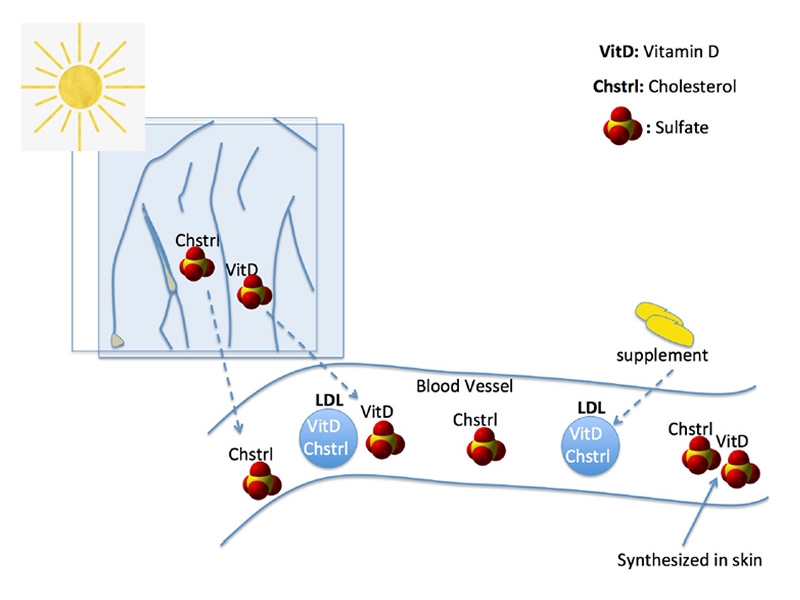
Stephanie Seneff
Figure 1: Schematic of the differences between sunlight exposure and vitamin D supplements. Cholesterol sulfate and vitamin D sulfate, synthesized in the skin following sunlight exposure, can be transported freely in the blood, rather than requiring carrier lipid particles like LDL.
Calcitriol is the 1,25(OH)-D3 that is usually produced by CYP enzymes in the kidney, and it is the “active form” of vitamin D. Kidney failure can derail this process, and so patients with kidney failure are often given calcitriol as a supplement. However, in a study published in 2006, it was found to be counterproductive to supplement young adults with childhood-onset end-stage renal disease with calictriol, because it is taken up by cells in the artery wall and leads to increased artery calcification.19 Basically, vitamin D mobilizes calcium, but it doesn’t control where calcium goes. I believe that sulfate deficiency in the vasculature drives a conversion of the smooth muscle cells into bone-like cells, and this causes them to actively take up calcium and phosphate. Vitamin D supplements will encourage them to do this faster. Artery calcification is one of the strongest risk factors for cardiovascular disease.
3.3 High Blood Pressure
A paper, aptly titled, “Sunlight Has Cardiovascular Benefits Independently of Vitamin D” argued that sunlight is a therapy option for high blood pressure, an important risk factor for cardiovascular disease.2 A scatter plot showing mean male population blood pressure vs. central latitude for a large number of countries, reproduced here as Figure 2, demonstrated a clear linear relationship. It was argued that the reason for the reduction in blood pressure was that sunlight stimulates the release of nitric oxide from the skin.
Population-blood-pressure-correlates-with-latitude.jpg
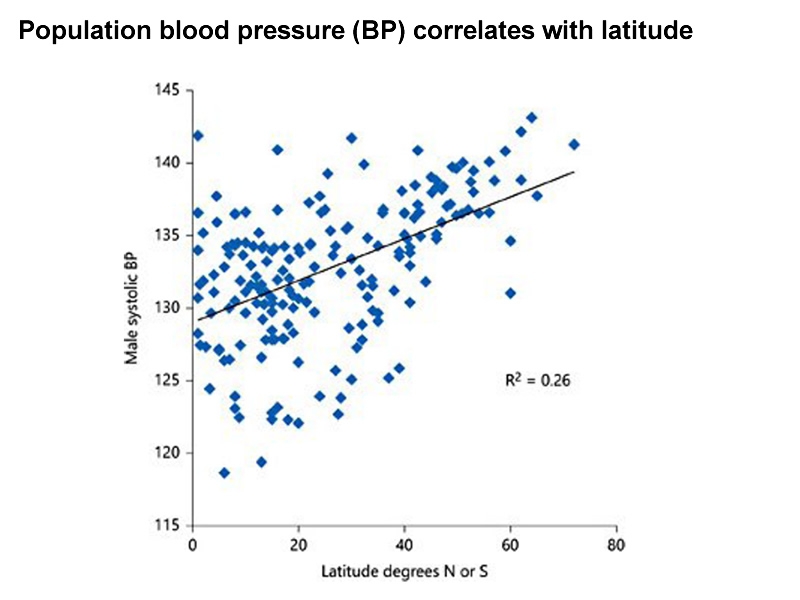
Stephanie Seneff
Figure 2: Population blood pressure (BP) correlates with latitude. Each point represents a country. Male systolic population BP is plotted against the latitude of the geographical mid-point of each country. BP values are from the MRC-HPA data in 1980. See Weller, 2016 for details [2].
Nitric oxide is a well-known “gasotransmitter,” a gaseous signaling molecule that has a remarkable ability to induce a relaxation of the artery wall and a resulting drop in blood pressure. Endothelial dysfunction linked to cardiovascular disease is associated with impaired production of NO from arginine by eNOS, and it causes high blood pressure.20 Researchers have recently become aware that the skin is somehow able to release nitric oxide in response to sunlight exposure. It is somewhat of a mystery exactly where the nitric oxide comes from, because it has become clear that it is not a result of direct synthesis by eNOS.21
A clue comes from the fact that glutathione reacts with nitric oxide to produce Snitrosoglutathione (GSNO), which I believe serves as a temporary storage form of NO. Almost miraculously, visible light (green, blue and purple) can catalyze the release of NO from glutathione.22 Not only does this cause a relaxation of the blood vessels, but it also frees up glutathione to react with hydrogen sulfide gas to produce sulfate. As illustrated in Figure 3, glutathione reacts with reduced sulfur to form glutathione persulfide (GSSH), and this can catalyze the oxidation of the extra sulfur atom to sulfur dioxide in the presence of superoxide. eNOS binds to flavins that respond to visible light by releasing electrons that convert oxygen to superoxide. The sulfur dioxide produced by eNOS is then oxidized to sulfate by sulfite oxidase. What this means is that the visible light in sunlight is crucial both for the release of NO from the skin and the synthesis of sulfate in the skin. And both of these results are crucial aspects of the beneficial effects of sunlight exposure. eNOS is a “moonlighting” enzyme that is able to switch between two synthesized products: nitric oxide and sulfur dioxide, depending on electromagnetic signaling that it receives from the circulating red blood cells, as described at length in a paper I published together with colleagues in 2015.23
These results might prompt medical professionals to advise people in higher latitudes to take a vitamin D supplement. However, a large study on vitamin D supplements and hip fractures gave disappointing results. The study involved women over 70 years old who had at least one self-reported risk factor for hip fracture (low body weight, previous fracture, maternal history of hip fracture, smoker, or poor health in general). To reduce the risk of vitaminosis D, women who took calcium supplements were excluded, as well as women with a history of bladder or kidney stones, renal failure or hypercalcemia. The intervention involved daily oral supplementation with 1000 mg calcium and 800 IU vitamin D3. Despite the near ideal experimental setup, after a median follow-up period of 25 months, there was no significant difference between fractures in the treatment group compared to the control group.
Visible-light-pathways.jpg
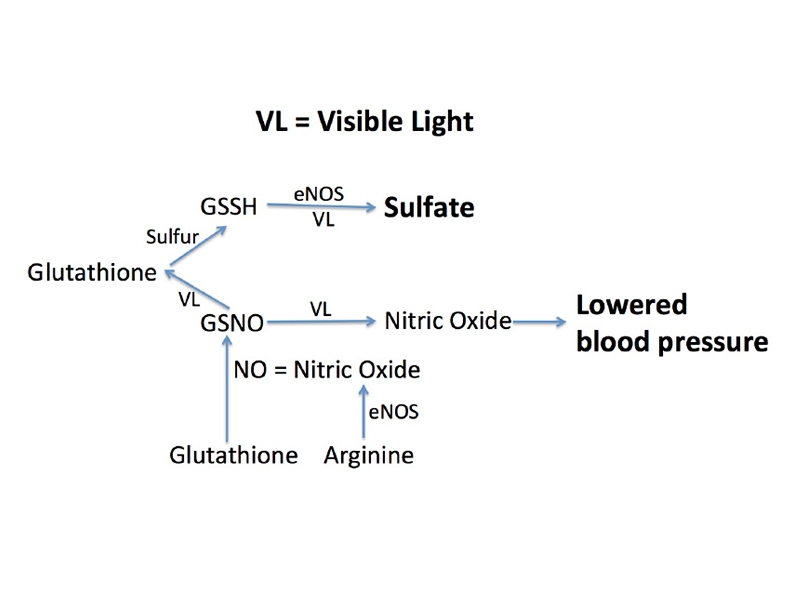
Stephanie Seneff
Figure 3: Pathways catalyzed by visible light that lead to synthesis of sulfate and release of nitric oxide from the skin, lowering blood pressure.
Another three-year study compared three different doses of vitamin D – 400 IU/day, 4,000 IU/day and 10,000 IU/day, specifically looking at bone density. Surprisingly, those on the highest dosage had statistically significantly worse outcome in terms of bone mineral density.26 I would argue that systemic sulfate deficiency is driving calcium into the arteries, leaching it from the bones, and excessive vitamin D increases the rate at which this happens.
4 Sunlight and the Eyes
We have been trained well by sunglass marketing ads to wear sunglasses whenever we go outside in order to protect our eyes from damaging UV rays. Melanin is what gives your eyes their color – blue, hazel, green, brown. It also protects them from UV rays. The human eye has evolved to naturally deal with sun exposure through antioxidant protection by melanin, as well as other antioxidant-defense systems based on glutathione and the enzyme superoxide dismutase (SOD). I believe it is crucial to get adequate sunlight exposure to the eyes, not just for the sake of the health of the eyes, but also because critical nuclei in the brain stem make good use of light that enters through the eyes.
4.1 The Pineal Gland and Sleep Disorder
The pineal gland sits behind the eyes and it can easily receive light that enters through the eyes. It plays an important role in circadian rhythms, and promotes restful sleep, by synthesizing large amounts of melatonin as the light fades in the evening. The melatonin is conjugated with sulfate and shipped out into the cerebrospinal fluid at night. In a paper published together with Wendy Morley, I have argued that melatonin supplies sulfate to the neurons in the brain at night, and that this supports the activities during sleep to break down and recycle cellular debris.27
A sulfotransferase enzyme is sharply upregulated during the daytime in the pineal gland, and it increases the amount of sulfate in the glycosaminoglycans in the intercellular spaces of the gland.28 This infers that sunlight catalyzes sulfate synthesis in the gland, and, indeed, the cells there express eNOS. The sulfate built up by day can be extracted from the matrix and conjugated to melatonin in the evening to maintain the brain’s supply of this critical nutrient.
4.2 The Substantia Nigra and Parkinson’s Disease
Parkinson’s disease is a relatively common progressive neurological disease manifested as a movement disorder, associated with tremors, stiffness and slowed movement. It is caused by a loss of neurons in the substantia nigra (“black substance”), a dark structure in the midbrain where dopamine is synthesized. The dark color is due to substantial production of neuromelanin, a close relative to the skin-tanning agent, melanin. Depigmentation of the substantia nigra due to loss of neuromelanin is a hallmark feature of Parkinson’s disease.29
A study comparing 186 patients with Parkinson’s disease with controls revealed that the PD patients had significantly lower bone density and significantly lower serum vitamin D levels compared to controls.30 Another study, based in China, compared 201 newly diagnosed patients with PD with 199 controls and also found that low serum vitamin D was linked to Parkinson’s.31 They also used a questionnaire to determine whether the study participants took vitamin D supplements and how much sun exposure they obtained. The frequency of Parkinson’s disease in the group in the highest quartile of sun exposure was only half of the rate for those in the lowest quartile. Interestingly, serum vitamin D levels were highly correlated with degree of sun exposure, but not with vitamin D supplementation.
One way in which sun exposure may be beneficial in Parkinson’s is through exposure to the eyes! Bright light therapy has been shown to benefit PD patients, both in improving sleep and mood, but also in improving motor function.32 A remarkable study on rats was able to measure the amount of light reaching the mesencephalon (midbrain, which houses the substantia nigra) when light was shone on the eyes.33 They demonstrated that a sharp peak was observed at around 710 nm, which is in the range of infrared light. It is likely that sunlight stimulates the synthesis of neuromelanin, just as it stimulates the synthesis of melanin in the skin. The neuromelanin then likely protects the dopaminergic neurons from oxidative damage, by mopping up free radicals.
Gerald Pollack’s research on structured “exclusion zone” water has shown that infrared light is very effective in growing the exclusion zone size, by as much as a factor of four. This will increase the mobilization of electrons (electricity) needed to oxidize oxygen and ultimately form sulfate, assisted by eNOS and sulfite oxidase. The sulfate is of direct benefit to form dopamine sulfate, the water-soluble form of dopamine that is easily transported and delivered to dopamine receptors, effecting movement. This story has parallels to the story regarding cholesterol sulfate in the skin.
5 Summary
Sunlight has been an important source of energy for planet earth since its inception. Plants have learned how to use the energy in sunlight to create organic matter. I believe that animals have exploited sunlight as a source of energy for movement and for cognition. Sulfate synthesis in the skin is a powerful way to capture the sun’s energy, and sulfate has diverse roles in the body that are essential for good health, particularly in maintaining a healthy vasculature, an electrical supply to the body, and an efficient delivery system for sulfate-conjugated biologically active molecules, such as cholesterol, vitamin D, dopamine and melatonin. Sunlight also offers natural protection from the harsh summer sun through the production of melatonin in the skin. Vitamin D supplements send the tissues a false signal that cholesterol sulfate is plentiful. These ideas are schematized in Figure 4.
Differences-between-vitaminD-through-supplements-or-sunlight.jpg
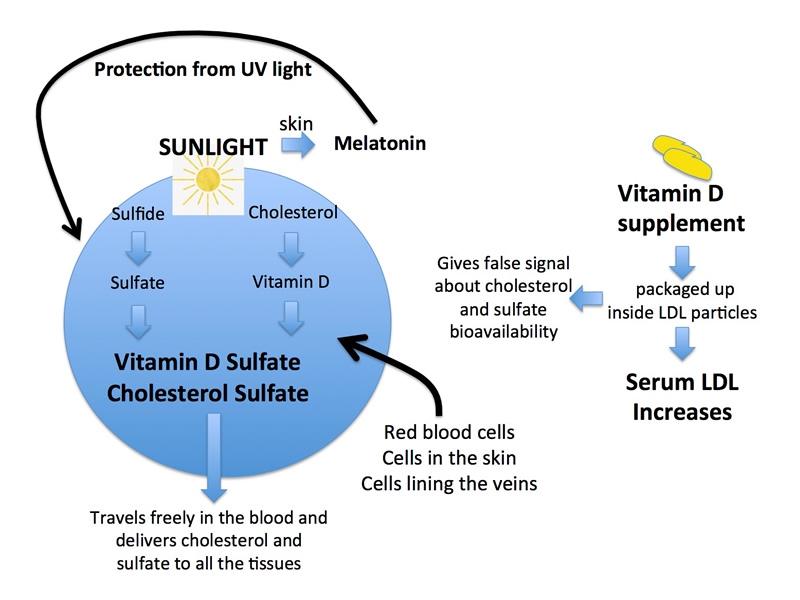
Stephanie Seneff
Figure 4: Schematic of differences between vitamin D supply through supplements or through sunlight exposure.
When I tell people that I worship the sun, they often respond with something like, “Yes, I am aware of all the myriad benefits of vitamin D to health.” Then, I have to explain that, no, it is not about vitamin D. It is about something vastly more important. Researchers are frustrated because they see that high serum vitamin D is associated with so many health benefits, yet, when they conduct the placebo-controlled studies on vitamin D supplements, they consistently yield disappointing results. When someone is diagnosed with skin cancer, they become intent on avoiding the sun, and worsen their prognosis. Sun exposure is important not just to the skin but also to the eyes, and, perhaps more importantly, to the structures in the brain stem behind the eyes that control circadian rhythms (pineal gland) and movement (substantia nigra).
Besides sunlight exposure, there are also some foods that naturally provide vitamin D and cholesterol sulfate, and these can be very important for people living in northern latitudes. I suspect that the eskimos got by by eating lots of seal blubber, an excellent source of both vitamin D and cholesterol sulfate. Other sources are raw milk and butter from grass-fed cows, organic lard, wild-caught fatty fish like salmon, and cod liver oil. But foods that are artificially supplemented with vitamin D won’t do the trick, because they don’t normally contain cholesterol sulfate. It’s also important to eat only certified organic foods, in order to minimize exposure to glyphosate and other toxic chemicals in the food that could disrupt the body’s ability to utilize sunlight appropriately.
There are some simple ways to increase your exposure to infrared light. One that I recommend is simply taking a bath with the water temperature set as high as you can comfortably stand. Add a half a cup of Epsom salts, and the sulfate in the Epsom salts will penetrate your skin, with the heat working synergistically to increase exclusion zone water. A sauna is another possibility, although there may be some issues there with electromagnetic field (EMF) exposure.
One of the best things that you can do to maintain good health is to walk barefoot in the water along the ocean shore on a sandy beach on a sunny day. The sand and water assure good grounding, providing the negative charge that is so important to mobilize electrons to fuel the structured water in the exclusion zone lining all the blood vessels. The ocean air is enriched in hydrogen sulfide gas that can easily penetrate the skin. If you don’t live near the ocean, walking outside barefoot in the grass is also beneficial. Even in winter when the sun’s rays are not so intense, the infrared light is still nearly as strong as in the summer. Even in the cold weather, winter sunlight shining on your face and hands is still health-promoting. Sunlight energizes the electrons in the exclusion zone to induce the synthesis of sulfate from sulfide, which, in turn, maintains the exclusion zone in a natural feedback loop. This is the electrical supply to the body, and sunlight is its primary source.
References
- David G Hoel and Frank R de Gruijl. Sun Exposure Public Health Directives. Int J Environ Res Public Health 2018; 15: 2794.
- RB Weller. Sunlight Has Cardiovascular Benefits Independently of Vitamin D. Blood Purification 2016; 41: 130-134.
- S. Seneff et al. Is Endothelial Nitric Oxide Synthase a Moonlighting Protein Whose Day Job is Cholesterol Sulfate Synthesis? Implications for Cholesterol Transport, Diabetes and Cardiovascular Disease. Entropy 2012; 14: 2492-2530.
- Binghua Chai et al. Effect of Radiant Energy on Near-Surface Water. J Phys Chem B 2009; 113(42): 13953-13958.
- Eleni Linos et al. Increasing Burden of Melanoma in the United States. J Invest Dermatol 2009; 129(7): 1666-1674.
- Haley N. Bray et al. Head and Neck Melanoma Incidence Trends in the Pediatric, Adolescent, and Young Adult Population of the United States and Canada, 1995-2014. JAMA Otolaryngol Head Neck Surg 2019; 145(11): 1064-1072.
- Philippe Autier et al. Melanoma and Use of Sunscreens: An EORTC Case-control Study in Germany, Belgium and France. International Journal of Cancer 1995; 61(6): 749-755.
- A Samsel and S Seneff, Glyphosate’s Suppression of Cytochrome P450 Enzymes and Amino Acid Biosynthesis by the Gut Microbiome: Pathways to Modern Diseases. Entropy 2013; 15: 1416-1463.
- M Berwick et al. Sun Exposure and Mortality from Melanoma. J Natl Cancer Inst 2005; 97(3): 195-9.
- Dmitriy Timerman et al. Vitamin D Deficiency is Associated with a Worse Prognosis in Metastatic Melanoma. Oncotarget 2017; 8(4): 6873-6882.
- JY Tang et al. Calcium Plus Vitamin D Supplementation and the Risk of Nonmelanoma and Melanoma Skin Cancer: Post Hoc Analyses of the Women’s Health Initiative Randomized Controlled Trial. J Clin Oncol 2011; 29(22): 3078-84.
- Yanqi Ye et al. A Melanin-Mediated Cancer Immunotherapy Patch. Sci Immunol 2017; 2: eaan5692.
- CF Garland and FC Garland. Do Sunlight and Vitamin D Reduce the Likelihood of Colon Cancer? Int J Epidemiol 1980; 9(3): 227-231.
- Grant WB. A Review of the Evidence Supporting the Vitamin D-Cancer Prevention Hypothesis in 2017. Anticancer Res. 2018 Feb;38(2):1121-1136.
- JE Manson et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Engl J Med 2019; 380(1): 33-44.
- M Feelisch et al. Is Sunlight Good for our Heart? European Heart Journal 2010; 31: 1041-1045.
- JP Pell and SM Cobbe. Seasonal Variations in Coronary Heart Disease. QJM: An International Journal of Medicine 1999; 92(12): 689-696.
- Vivek G Patwardhan et al. Randomized Control Trial Assessing Impact of Increased Sunlight Exposure versus Vitamin D Supplementation on Lipid Profile in Indian Vitamin D Deficient Men. Indian J Endocrinol Metab 2017; 21(3): 393-398.
- S Briese Arterial and Cardiac Disease in Young Adults with Childhood-Onset End-Stage Renal Disease – Impact of Calcium and Vitamin D Therapy. Nephrol Dial Transplant 2006; 21: 1906-1914.
- P Puddu et al. Endothelial Dysfunction in Hypertension. Acta Cardiol 2000; 55(4): 221-32.
- D Liu et al. UVA Irradiation of Human Skin Vasodilates Arterial Vasculature and Lowers Blood Pressure Independently of Nitric Oxide Synthase. J Invest Dermatol 2014 134: 1839-1846.
- Daniel J Sexton et al. Visible Light Photochemical Release of Nitric Oxide from S-Nitrosoglutathione: Potential Photochemotherapeutic Applications. Photochem Photobiol 1994; 59(4): 463-7.
- S Seneff et al. A Novel Hypothesis for Atherosclerosis as a Cholesterol Sulfate Deficiency Syndrome. Theoretical Biology and Medical Modeling 2015; 12: 9.
- O Johnell et al. Latitude, Socioeconomic Prosperity, Mobile Phones and Hip Fracture Risk. Osteoporosis International 2007; 18(3): 333-337.
- Rani Ramason et al. Prevalence of Vitamin D Deficiency in Patients With Hip Fracture Seen in an Orthogeriatric Service in Sunny Singapore. Geriatr Orthop Surg Rehabil 2014; 5(2): 82-86.
- Lauren A Burt et al. Effect of High-Dose Vitamin D Supplementation on Volumetric Bone Density and Bone Strength: A Randomized Clinical Trial. JAMA 2019; 322(8): 736-745.
- WA Morley and S Seneff. Diminished Brain Resilience Syndrome: A Modern Day Neurological Pathology of Increased Susceptibility to Mild Brain Trauma, Concussion, and Downstream Neurodegeneration. Surgical Neurology International 2014; 5: 97.
- B Kuberan et al. Light-Induced 3-O-Sulfotransferase Expression Alters Pineal Heparan Sulfate Fine Structure: A Surprising Link to Circadian Rhythm. JBC 2004; 279(7): 5053-5054.
- Robert L Haining et al. Neuromelanin, One of the Most Overlooked Molecules in Modern Medicine, is Not a Spectator. Neural Regen Res 2017; 12(3): 372-375.
- F van den Bos et al. Bone Mineral Density and Vitamin D Status in Parkinson’s Disease Patients. J Neurol 2013; 260(3): 754-60.
- Juan Wang et al. Vitamin D and Sunlight Exposure in Newly-Diagnosed Parkinson’s Disease. Nutrients 2016; 8(3): 142.
- S Rutten et al. Bright Light Therapy in Parkinson’s Disease: An Overview of the Background and Evidence. Parkinson’s Disease 2012; Article ID 767105.
- Stefania Romeo et al. Eyes as Gateways for Environmental Light to the Substantia Nigra: Relevance in Parkinson’s Disease. Scientific World Journal 2014: 317879.
Sunlight and Vitamin D: They’re Not the Same Thing! was originally published in Masters of Health Magazine, October 2020. Used with permission.


