Pelvic pain is not caused by a deficiency of the birth control pill
Fact!
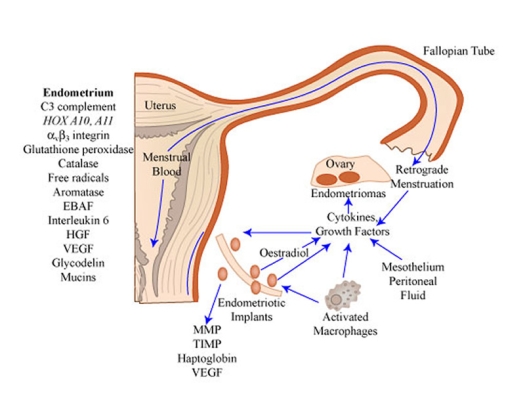
Pelvic pain is not caused by a deficiency of the birth control pill. March is #endometriosisawareness month so let’s break this down. Endometriosis is a painful condition in women where tissue that is similar to uterine tissue lives outside the uterus around other pelvic organs.
Endometrial tissue responds to the hormonal changes of the menstrual cycle so that it can cause:
- Painful periods
- Pain during intimacy
- Pain with bowel movements
- Pain during urination
- Fertility problems
But here’s the thing. Standard treatments for endometriosis are the birth control pill (or other hormonal therapies) and sometimes surgery. Don’t get me wrong – some women benefit from these treatments and they can be part of the overall plan. The problem is this:
The birth control pill does not treat the root cause of the issue
That means that many women continue to struggle with pain even with the “best” treatments. Do you want to know what the real causes of endometriosis and pelvic pain might be? Because that’s what functional medicine is all about. We find the cause.
4 Root Causes of Pelvic Pain
Have you ever wondered if there might be other ways to deal with endometriosis and pelvic pain than to just take the birth control pill? Then keep reading. Even though the causes and contributing factors are unique to each woman dealing with pelvic pain, there are common causes we can investigate with functional medicine. For example:
- Hormone Imbalance: Some women with endometriosis have estrogen dominance, or a mismatch between the amount of estrogen and progesterone produced. How is this tested? Hormone testing.
- Gut Microbiome: Research has found unique changes in the gut microbiome associated with endometriosis. How is this tested? Stool tests.
- Immune Reactions: Higher concentrations of inflammatory molecules and immune cells are found in endometrial tissues, suggesting immune reactions may be at play. How is this tested? Blood tests.
- Chemicals & Toxins: Common everyday products like plastics and lotions often contain endocrine-disrupting chemicals that mess with your hormones and can contribute to endometriosis and pelvic pain. How is this tested? An environmental toxin panel.
4 Lifestyle Tips for Pelvic Pain
All the lifestyle changes in the world will not correct the problem if the cause is not identified. Here are some lifestyle changes that many women have found helpful.
Eat an Anti-Inflammatory Diet
No matter the cause, inflammation is almost always at play in women struggling with pelvic pain. Focusing on omega-3 fats and lots of antioxidant-rich fruits and vegetables can lessen the stress on your immune system.
Workout to Sweat
Working out can increase your endorphins to decrease sensitivity to pain. Exercise supports hormonal balance, and sweating helps to clear toxins from the body.
Cut Alcohol
Alcohol can increase estrogen levels and place a burden on your detoxification systems. For whatever temporary benefits you feel, there’s a good chance it will make things worse in the long run.
Practice Deep Breathing
Pain can be stressful, and stress can make pain worse in a vicious cycle. Deep breathing, yoga, or meditation are great ways to relieve stress.
13 Supplements Studied in Pelvic Pain
A recent review looked at studies of nutritional supplements in the context of endometriosis and chronic pelvic pain.
13 supplements showed promise:
- Vitamin D
- Zinc
- Omega-3s
- Curcumin
- Quercetin
- N-acetylcysteine (NAC)
- Probiotics or Prebiotics
- Resveratrol
- Alpha-lipoic acid (ALA)
- Vitamin C
- Vitamin E
- Selenium
- EGCG (from green tea)
Does this mean that every woman with pelvic pain should go purchase all of these supplements? No. Pelvic pain is complicated and needs to be evaluated by a qualified healthcare practitioner and then additional testing can be done to understand the root cause. It is possible to tailor a targeted plan that often includes supplements – but not a laundry list like this.
Revised by Joanne Quinn, PhD; content provided by Wellnesswriter.com.