TheHerxheimerEffectPybusDaviesObservations.jpg
Dr. Paul K. Pybus
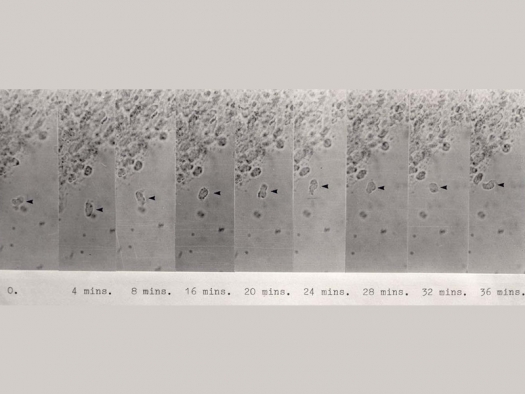
Synovial fluid after 4 days standing at room temperature, under the high power field. The exposures were taken at four minute intervals. It will be seen that the rate of progress of the amoeba (arrowed) is extremely slow, about 20µ per hour.
Introduction
Dr. Paul Pybus, a surgeon and Englishman who resided in South Africa, was my friend and former Chief Medical Advisor for The Rheumatoid Disease Foundation.
In the 1960s he worked with Roger Wyburn-Mason, M.D. the man who brought us our first consistently successful treatment for otherwise crippling arthritis.
From early teachings by his mentor, Wyburn-Mason, Paul Pybus developed our technique of intraneural injections that is so successful for the pain of both Osteoarthritis and Rheumatoid Arthritis, and which may be the foundation for explaining one of the causative factors of Osteoarthritis. That story is elsewhere.13
An article prepared by Dr. Paul Pybus at the same time as the above mentioned Intraneural Injections... booklet was titled “The Herxheimer Reaction History” (see below). Paul prepared this material because of the extreme importance of noting and accounting for the Herxheimer effect when treating arthritics. It is a pity that many modern-day physicians have not been taught the Herxheimer, or, if they have, do not understand its importance when treating a number of diseases.
It is a phenomena that results when there is an intensification of the disease symptoms and often an expansion of similar symptoms to other places all of a temporary nature, after which the patient is improved or well. Often it appears to some as if they have the flu, and so is described as “the patient having flu-like symptoms.” “Flu-like symptoms” is an over-simplification of what happens in varying cases and with varying patients.
When treating Leishmaniasis, Syphilis or Tuberculosis, the phenomena is called Herxheimer, when treating Leprosy it’s called Lucio’s Phenomena. Other rare tropical diseases also call it the Herxheimer. When treating Candidiasis, patient’s and doctors call it the “die-off effect.”
In all cases of the Herxheimer, there is the appearance of a war or tussle going on inside the body akin to the antigen/antibody warfare, where the body produces fever, sweat, aching and swollen joints, diarrhea, nausea, and so on, in varying proportions with varying degrees depending upon state of metabolism, genetics, source of disturbance and so on.
It is my belief that some prescription drugs wrongly are described to be toxic in a certain way because, on observing an Herxheimer reaction in the patient trying the new drug, the drug researchers (and others’ observations during subsequent follow-on research and use of the drug) do not fully understand the Herxheimer and believe the cause is the drug’s “toxicity.” Even with a full understanding of the Herxheimer effect, a pharmaceutical company must follow the “rule of over-caution,” to satisfy FDA requirements for the “health and safety” of us more ignorant citizens. Thus, even with knowledge of the Herxheimer effect, a physician researcher is not necessarily in a position whereby he can, or wants to, discriminate between drug toxicity and the Herxheimer effect.
It is necessary for the successful treatment of Rheumatoid Diseases, therefore, that a physician attend the patient who uses our treatment protocol, and that the physician fully comprehend the distinctions between specific drug toxicities and the Herxheimer effect. This distinction probably can come only through the experiences of applied clinical practices.
Drugs do have toxicities of their own, but the essential importance for Rheumatoid Arthritics is to be able to discriminate between the two: Herxheimer effect and toxicity.
This is unfortunate, as it clouds otherwise desirable treatment modes, not just those recommended in our treatment protocols for arthritics. From another viewpoint, those who fully understand the distinction between the Herxheimer effect and drug toxicities find themselves with a guiding clinical tool that permits the physician early in the treatment regime to determine the probability of success for a given patient.
Through our Physicians, we have learned that, generally speaking, the more severe the induced Herxheimer, the more probability of wellness — which is not to say that one who has a very light Herxheimer may not also get well.
Prior to Dr. Paul Pybus’ work developing intraneural injections, it was felt that Osteoarthritis and Rheumatoid Arthritis had little in common, except that here and there folks with Rheumatoid Arthritis might also have some Osteoarthritis.
Perhaps it is still true, that the causes are indeed distinguishable.
But one very interesting set of experiences has come forth from the application of the Wyburn-Mason/Pybus/Prosch Intraneural Treatment on both Rheumatoid and Osteo victims: joint pain and joint damage in both diseases seem to stem from the same source, namely a disturbance in certain key trigger points along the peripheral nervous system. The peripheral nerves are usually those nerves close to the surface of the body, and have no insulative layers — similar to an electric wire passing current without insulation — called the C fibers, or “unmyelinated” fibers.
It might very well be that Osteoarthritis can be halted with Pybus’ intraneurals, along with good diet, including proper supplements, hormones and changes in life style.
Those possibilities, along with Pybus’ Intraneural injections are told elsewhere in our literature.
The Herxheimer Reaction History
by Dr. Paul K. Pybus, M.A., M.B., B. Chir (Cambridge), M.R.C.S., M.R.C.P. (London), D.R.C.G. (London) F.R.C.S. (England)
This reaction was first described by an Austrian dermatologist Jarisch Adolf Herxheimer10 working in Vienna and Innsbruck in 1895 and shortly after this, confirmed by his brother Karl Herxheimer1,2 also a dermatologist working in Frankfort.
They were both mainly called upon to treat syphilitic lesions of skin by means of mercury and later arsenical and bismuth preparations. They both noticed that when treating these patients many of them developed signs of high fever, profuse perspiration, night sweats, nausea and vomiting. What was more they also observed that the skin lesions became larger and inflamed before settling down and healing. In addition they found that those cases that responded in this most violent manner healed the best and fastest. The patient was quite ill for 2-3 days after which the syphilitic lesions resolved.
Jarisch Herxheimer accounted for this reaction as a toxic manifestation caused by the foreign proteins released from the dying spirocheates. Meanwhile his brother Karl1,2 described in detail the Herxheimer fever. There is first a febrile phase with pyrexia, malaise and often a sore throat. The lesions are then aggravated and the ash if present becomes more marked with tension in the regional lymph nodes being more pronounced. In addition the primary ulcer would become oedematous and painful (the primary chancre is characterized by its painlessness). [In a letter to The Lancet, p. 340, Feb. 12, 1977, it is suggested that two of the three identifying features of a Herxheimer were known since the end of the 15th century when arsenical ointment was first used to treat the great pox which had just arrived in Europe from the New World: Ed.]
During this reaction many other signs appeared such as histologic changes such as transient acute inflammation in the lesion, a leucocytosis and lymphopaenia which was greatest as the pyrexia was at its zenith.
It was suggested by another surgeon Heyman8 that these histologic changes indicate that the reaction was hypersensitivity pehnomenon of the delayed type similar to the tuberculin hypersensitivity type of reaction.
Theories as to Cause
- Herxheimer et al.1,2,10 The phenomenon is caused by the release of endotoxin of spirochaetal breakdown products following treatment. These products are reacting with sensitized syphilitic tissue to produce exacerbation of the lesion.
- Milian.3 Suggested it was due to stimulation of the spirochaetes and inadequate medication. [Bradford and Allen state that "The purpose of endotoxin to the bacterium that produces it is to act as a semipermeable membrane, limiting and regulating the nature of substances that may enter and provide nutrient for that organism. for this reason endotoxins reside solely on or near the surface (cell wall) and are shed into the surrounding medium only upon the death of the organism. This fact may well be an explanation for what has become known as the Herxheimer reaction in which a patient becomes worse following the administraiton of anti-biotics or other form of treatment that kills the causative organism.20]
- Jadassohn.9 Suggested that the direct effect of the antisyphilitic drug on the tissue was an entirely toxic reaction.
- Fleishman.4 Suggested this reaction was of a vascular reflex mediated by the autonomic nervous system.
In 1943 Mahoney et al5 first described Jarisch Herxheimer Reaction in syphilitic patients treated with penicillin and since then it has been observed that other chemotherapeutic agents that are effective with syphilis also produce a Herxheimer reaction.
Moore et al6 regard the reaction as all or none phenomenon but it was found that if the dose was less than 10 international units per kilogram bodyweight the reaction did not occur. The increase of the dose, however, did not increase the degree of the reaction. It also occurred equally in the seropositive and seronegative patient.
Joulia et al7 reported that during the Jarisch Herxheimer reaction the eosinophils decreased showing it to be an antigen antibody reaction. However, Heyman found that using antihistamines had no effect on the reaction whatsoever.
The Jarisch Herxheimer reaction occurs in other diseases treated with anitbiotics. It has been noted in:
- Yaws treated with penicillin.
- Vincents Angina treated with metronidazole.
- Relapsing fever (also a spirochaetal disease) treated with tetracycline.
- Rat bite fever (also due to a spirillum) treated with penicillin or tetracycline.
- Leprosy where it is known as the Lucia phenomenon treated with Dapsone.
- Brucellosis treated with chloramphenicol.
- Glanders treated with erythromycin.
- Anthrax treated with aureomycin.
- Rheumatoid Disease treated with metronidazole [and other drugs: Ed.]
- Psoriasis treated with metronidazole [and other drugs: Ed.]
- [Systemic Lupus Erythematosus and Scleroderma treated with metronidazole and other drugs: Ed.]
In 1972 Gudjonsson11 investigated the Herxheimer reaction in adult seropositive and negative syphilitics and found a febrile reaction in 60%. It could be produced with doses above 10 International units per kilogram. However, in 30% of cases no reaction occurred until as much as 600,000 I.U. per kg, were given and so it would appear that the higher doses produced a stronger reaction than the lower ones and this was at variance with the observations of Moore.
He also noted an increase in the neutrophils and a decrease in the lymphocyte count which occurs when the temperature is greatest. The Eosinophil decreased and may be due to the de-granulation of their cells as they phagacytose the breakdown products of the treponemes. This is also an observation in my own series of treated rheumatoid arthritic cases with metronidazole as the eosinophils are completely removed from the blood in most cases with a positive Herxheimer reaction.
Effect of Prednisone on Herxheimer reaction. Here the Prednisone clearly influences the febrile response at a daily dose of 40 mg. The leucocyte changes are not effected and so the Prednisone influences only the febrile component and not the other manifestations of the reaction. Gudjonsson concludes that the reaction is not of an allergic nature, but is caused by some leucocyte pyrogen released by phagocytosis of the treponemes.
Discussion
If we say that Gudjonsson is correct and that the reaction is due to the release by the leucocytes of a pyrogen when something is phagocytosed, then this further suggests that the Herxheimer reaction seen when treating rheumatoid arthritis with certain drugs, is due to the phagocytosis of an infective agent. Thus, although no one apart from Stamm and Wyburn-Mason12 have found amoebae for certain, this is strong evidence for an infective cause of the disease. An Herxheimer reaction is the one constant finding in all our search and the strength of the reaction correlates very closely to clinical improvement as shown separately by Prosch, Bingham and Pybus13 [and now others: Ed.].
Furthermore in my own recent series the correlation is shown to be 100% correct.
I have also shown what would occur should these cases that I have done be analyzed on a double-blind study by someone who was not acquainted with the Herxheimer reaction.
Herxheimer reaction is becoming the cornerstone of our present research and unless full account is taken of its occurrence any double-blind trial performed will tend to be misleading. The mere fact that it occurs will influence any such trial and would probably be more advantageous if the final assessor could be suitably blinded as to the previous occurrences of the Herxheimer reaction.
I had sincerely hoped that this was being done at our double-blind studies. I have strongly advocated that it be done. [The Herxheimer reaction was not taken into account at our double-blind studies at Bowman Gray School of Medicine. This study was reported separately: Ed.]
The symptoms of the Herxheimer can be most severe. They can discourage not only the patient, but also the doctor and anyone running a trial not knowing of these, will assume they are toxic symptoms and remove the patient from the trial [as occurred at our Bowman Gray School of Medicine study on use of Clotrimazole: Ed.].
This also occurred in the original Guy’s18 trial when they came to the conclusion that metronidazole had no effect on rheumatoid arthritis and this lack of recognition of the Herxheimer reaction did untold damage to our cause. Not only were the numbers in the trial inadequate, only 20, but other medications were not stopped [Nonsteroidal anti-inflammatories: Ed.]. Follow up was only for 6 weeks (they should have waited at least two months), strike dosage was usually inadequate either to produce an Herxheimer or clinical improvement (400 mg b.d.) and the one case that did produce a reaction was withdrawn because of these ‘side effects.’ [The Herxheimer effect: Ed.].
Recent Progress
This year I have made an analysis of 24 cases of Rheumatoid Arthritis (RA) and this revealed many interesting facts.
In a total of 288 metronidazole nights there were only 47 nights or 16.32% when nothing happened at all. All the rest (241 or 83.68%) showed some reaction and were divided up according to the following:
- Heavy perspiration and night sweats: 54
- Flu-like symptoms:47
- Rigors:32
- Fever:2
- Headaches:85
- Malaise:43
- Diarrhea:19
- Nausea:49
- Vomiting:8
- Pain in other joints previously unaffected:79
- Burning micturition:21
- Bone pain:39
- Itching:33
- Flushing of skin and red patches:39
These figures are all the more remarkable when one considers that in the normal person without rheumatoid disease, this dose of metronidazole produces no symptoms whatsoever.
Thus, in our campaign in the treatment of rheumatoid disease, two points stand out markedly:
- Metronidazole and our other recommended medicines work;
- That a Herxheimer reaction occurs in at least 83% of metronidazole nights.
These two points seem to prove that an infection must be at least at the root of the rheumatoid disease problem.
[I find it most interesting — and consistent — that Dr. Pybus found 83% suffer a Herxheimer reaction, and subsequently show improvement or alleviation of this disease, and that Gus Prosch, Jr.,14 M.D. has shown a cure/remission rate of about 80% since 1982, using these oral medications combined with intraneurals and proper diet: Ed.]
[It is stated and referenced in Roger Wyburn-Mason’s12 various works that The Herxheimer response only occurs when an organism more complex than a bacillus is being killed by an antibiotic and due to the Herxheimer, this fact “proves” that the infective agent must be of a complicated structure. Ed.]
In South Africa, our research has been based on the effect of metronidazole on moving cells found in joint fluid. It has been shown that the macrophage-like cells found in the rheumatoid fluid, when challenged with metronidazole, first respond with an increased movement of a writhing character. These movements after 15 minutes largely subside to be replaced by the slower movement and eventually after 309 minutes they are mostly crenated and absorbed. Thus, the metronidazole would appear to kill the macrophage [in vitro: Ed.].
Wyburn-Mason stressed that the Amoeba chromatosa was often confused with macrophages, and that they had the power of independent existence for a long time, which fact some of us have corroborated.[He may have viewed clusters of cell-wall deficient bacteria: Ed.]
Kwang Jeon15 [University of Tennessee, U.S.A.] cultured these cells in joint fluid that were up to one week old and showed that they would develop into fibroblasts. However, the fluid that had been treated with metronidazole grew nothing.
Davies16 has noted these macrophages in penassy fluid left at room temperature were still fresh (active) for as long as 24 days.
Wyburn-Mason17 described the macrophage in great detail and gave it great prominence in his book on the reticuloendothelial system. He concluded it was not mesodermal in origin as is so often claimed and said, but not proved, to develop from the monocyte, but rather was it neuroectodermal in origin and was developed from the trophic nerve ending.
Later, when working with Stamm,12 he was convinced that these were in all probability amoebae. Furthermore, they both claimed that they had cultured them, but attempts by all of us have failed to repeat this.
However, these macrophages have been grown at the University of Tennessee by Kwang Jeon and this, I feel, is a great step forward.
For those who are interested in pursing the easing of the Herxheimer, the following suggestions have made made, in addition to various traditional allopathic remedies.
As the "die-off effect" is the same as the well-known Herxheimer effect, one might also ease the pain of temporarily increasing toxins by use of a steam (dry or hot) sauna.
Russ McMillan, D.D.S., D.P.H., Dr. P.H. suggests "something that helps with the rather debilitating symptoms that accompany the Herxheimer effect after medication. I take a saltz bath which consists of adding 1 cup salt, 1 cup soda, 1 cup epsom salts, 1 cup aloe vera, to a hot bath which I remain in and keep hot for about 1-1/2 hours all the while consuming about 2 quarts of warm water. Evidently the perspiration and osmotic pressure removes the causative toxins. I find it quite helpful.19
References
- Herxheimer, K. Krause: “Uber eine bei Syphilitische vorkommende Quecksilerberreaktion. Deutsch. Med. Wschr. 28:50, 1902.
- Herxheimer, K. and Martin, H.: So-called Herxheimer reactions. Arch. Derm. Syph. 13:115, 1926.
- Millian, G.: Syphilis: Reaction d’ Herxheimer. Biotropisme. Paris nd.: 37:91, 1920.
- Fleishman, K. and Kreibich, C.: Zum Wesen der Reaktion nach Jarish-Herxheimer. Me. Klin. 21:1157, 1925.
- Mahoney, J.F., Arnold, R.C., and Harris, A.: Penicillin treatment of early syphilis. Amer. J. Public Health 33:1387, 1943.
- Moore, J.E., Farmer, T.W. and Hoekenga, M.T.: Penicillin and the Jarisch-Herxheimer reaction in early, cardiovasculaar and nuerosyphilis. rans. Ass. Amer. Phycns. 61:176, 1948.
- Joulia, P., Pautrizell, R., Texier, L. and Sebra, De.: La chute des eosinophiles sanguines apre une premiere injeciton de penicilline au cours de la syphilis primo-secondaire: temoin du conflit antigene-anticorps. ull. Soc. Franc. Derm. Syph. 58:399, 1951.
- Heyman, A., Sheldon, W.H. and Evans, L.D.: Pathogenesis of the Jarisch-Herxheimer reaction. rit. J. vener. Dis. 28:50, 1952.
- Jadassohn, J.: Beitrag zur Jarisch-Herxheimer Reaktion. Z. Haut Geschlechtskr 19:158, 1965.
- Jarisch, A. Wien. med Wschr. 45:721, 1895.
- Gudjonsson, Haraldur: The Jarisch-Herxheimer Reaction, Stockholm 1972 (A summary based on the following seven publications:
- Skok, E. and Gudjonsson, H.: On the allergic origin of the jarisch-Herxheimer reaction. Acta Dermatovfener (Stockholm) 46:136, 1966.
- Gudjonsson, H. and Skog, E.: The effect of prednisolone on the Jarisch-Herxheimer reaction. Acta Dermatovener (Stockholm) 48:15, 1968.
- Gudjonsson, H. and Skog, E.: Fever after inoculation of rabbits with Treponema pallidum. Jarisch-Herxheimer reaction? Proc. 18. Meeting Scand. Dermatol. Ass., Turku 1968.
- Gudjonsson, H. and Skog, E.: Fever after inoculation of rabbits with Treponema pallidum. Brit. J. vener. Dis. 46:318, 1970.
- Gudjonsson, H., Newman, B. and Turner, T.B.: Demonstration of a virus-like agent contaiminating amterial containing the Stockholm substrain of the Nichols pathogenic Treponema pallidum. Brit. J. vener. Dis. 46:435, 1970.
- Gudjonsson, H. Newman, B. and Turner, T.B.: Screening out a virus-like agent from the testicular suspension of the Nichols pathogenic Treponema pallidum. Brit. J. vener. Dis. In press at time summary was written.
- Gudjonsson, H.: Experiments to induce febrile Jarisch-Herxheimer reaction on syphilitic rabbits with penicillin and erythromycin. Acta Dermatovener. (Stockholm). In press at time summary was written.
- Wyburn-Mason, Roger: The Causation of Rheumatoid Disease and Many Human Cancers, IJI Publishing Co., Ltd., Tokyo, Japan, 1978. [Summary available through The Rheumatoid Disease Foundation, Rt. 4, Box 137, Franklin, TN 37064, same title.]
- Arthritis: Osteoarthritis and Rheumatoid Disease Including Rheumatoid Arthritis, Anthony di Fabio, & Gus J. Prosch, Jr., M.D., Rheumatoid Diseases Cured at Last (1985); Anthony di Fabio, The Art of Getting Well, Anthony di Fabio (1988); Intraneural Injections for Rheumatoid Arthritis and Osteoarthritis & The Control of Pain in Arthritis of the Knee, Dr. Paul K. Pybus, (1989), The Arthritis Trust of America/The Rheumatoid Disease Foundation, 7376 Walker Road, Fairview, TN 37062-8141
- Prosch, Gus J., Jr.: Personal communcation: Ed.
- Jeon, Kwang: Research proposal and paper (based on arthritic knee effusion samples submitted by our referral physicians from their patients) submitted to The Rheumatoid Disease Foundation.
- Pybus, Paul K. P, Davies, A.H.: Paper submitted to The Rheumatoid Disease Foundation (based on knee effusions submitted by our referral physicians.)
- Wyburn-Mason, Roger: The Reticulo-Endothellial System in Growth and Tumour Formation, Henry Kimpton, London, England, 1958.
- Guy [study performed in South Africa by a Rheumatologist], reference source lost.
- Personal letter from Russ McMillan, D.D.S., M.P.H., Dr. P.H. to The Arthritis Trust of America/The Rheumatoid Disease Foundation, June 13, 1994.
- Robert W. Bradford, D.Sc., Henry Allen, "The HLB Blood Test as an Indicator of Oxidative Injry & Disseminated Intravascular Coagulation," Townsend Letter for Doctors, 911 Tyler Street, Port Townsend, WA 98368-6541, April 1995, p. 30. [From Morrison, D.C., et. al., The effects of bacterial endotoxins on host mediation systems, American Journal of Pathology 93 526 (1978).]
Authors of contributions/quotations are alphabetically arranged; major author, if any, is in bold.
- Henry W. Allen
- Robert W. Bradford, D.Sc.
- Dr. A.H. Davies
- K. Fleishman
- Haraldur Gudjonsson
- Adolf Herxheimer
- Dr. Karl Herxheimer
- Dr. A. Heyman
- J. Jadassohn
- Dr. Jarisch
- Kwang Jeon, Ph.D.
- P. Joulia
- J.F. Mahoney
- Russ McMillan, D.D.S., M.P.H.
- Dr. P.H., G. Milian
- J.E. Moore
- Gus J. Prosch, Jr., M.D.
- Dr. Paul K. Pybus
- Vice Admiral Stamm
- Roger Wyburn-Mason, M.D., Ph.D.
- Responsible editor/writer Anthony di Fabio.
Copyright 1991. All rights reserved by The Roger Wyburn-Mason and Jack M. Blount Foundation for the Eradication of Rheumatoid Disease AKA The Arthritis Trust of America.
The Rheumatoid Disease Foundation / The Arthritis Trust of America was dissolved in 2020 and all website content was transferred to the Foundation for Alternative and Integrative Medicine.


