GERD-stomach-illustration.jpg
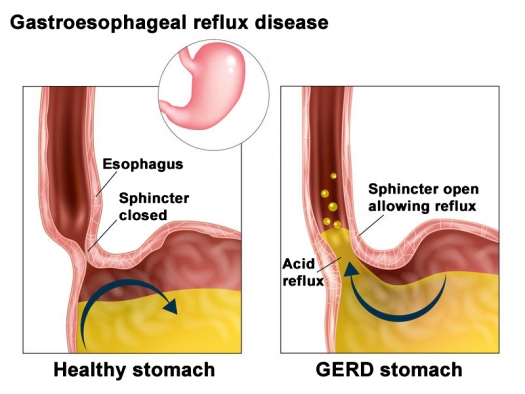
Illustration by Viktoriia Kasyanyuk / 123rf.com
We’re all aware – especially women – of menopause, when women’s ovaries reduce and then stop secreting estrogens, progesterone, and a bit of testosterone. Men’s testosterone levels decline with time (a process termed “andropause”) of course much more slowly than women, but since all of our bodies have been saturated with thousands of pesticides, herbicides, and other killer molecules never, ever present on planet Earth before the “20th century,” men’s testosterone levels have started to decline at significantly earlier ages than ever before. Many more men have become more aware of andropause at significantly younger ages than all of their male ancestors.
Since the beginnings of comprehensive bio-identical hormone therapy (“BHRT,” which was first done at Tahoma Clinic in the early 1980s), literally hundreds of thousands of post-menopausal women have observed that they’re staying healthier for significantly longer than post-menopausal women not using BHRT. As “bonus points,” most post-menopausal women using BHRT for a decade or more have noticed that they don’t appear to be aging at the same rate as post-menopausal women of the same age not using BHRT.
We men are (as women sometimes say) slower than women to actively take care of our own health. However, we are faster – for obvious-to-men reasons – to do something about our declining testosterone levels, and doing that as part of male BHRT has the same effectiveness in promoting healthy longevity as BHRT does for women.
There’s a third important “pause” that happens to both women and men that very significantly lowers our chances of healthy longevity. This third “pause” is totally overlooked and (believe it or not) often actually made much worse by “mainstream” or “standard of care” medicine. This third “pause” is “Gastropause,” which is the often-declining function of our stomachs over time. “Gastropause” doesn’t happen to everyone – at Tahoma Clinic we’ve congratulated the occasional 85 year old about his or her 100% normal stomach function – but more often than not, Gastropause occurs significantly before that age.
“Gastropause” (although that name wasn’t used then) was extremely well documented in a 1932 research publication from the Mayo Clinic titled “Normal Range of Gastric Acidity from Youth to Old Age” published in 1932.1 Led by Drs. Frances Vanzant and Walter C. Alvarez, Mayo Clinic researchers reviewed stomach acid secretion tests done for 3,308 research volunteers... 1,454 women and 1,854 men… between the ages of twenty and seventy-nine years old. (They added to their own data statistics from similar studies done with 365 children ages one to twenty, with the total reviewed being 3,673.)
Here’s their report about the percentage of individuals 20 years of age and older whose stomachs were found to secrete suboptimal hydrochloric acid, the definition of “Gastropause.”
As might be expected, the frequency of the problem increased in both sexes with age until ages sixty to sixty-nine. Women had a higher percentage of sub-optimal stomach acid secretion (“hypochlorhydria,” or lower than optimal stomach acid, and “achlorhydria,” no secretion of acid) than men in every age group. Here is a summary of what the researchers reported:
| Age | Men | Women |
|---|---|---|
| 29-29 | 5.7% | 10.8% |
| 30-39 | 8.0% | 21.0% |
| 40-49 | 22.7% | 32.6% |
| 50-59 | 38.3% | 40.9% |
| 60-69 | 49.8% | 59.2% |
| 70-79 | 42.2% | 35.5% |
The researchers give a possible explanation for the decline in the percentage of individuals tested with low or no stomach acid in their 70s: “After the age of 65 years there appears to be a definite falling off in the amount of [hypochlorhydria and] achlorhydria, possibly because persons with [hypochlorhydria and] achlorhydria are not as hardy or long-lived as are those who have a strongly acid gastric juice.” A briefer version of this explanation would be: “Individuals with low or no stomach acid don’t live as long!”
Good digestion starts with stomach acid! The same cells that make hydrochloric acid make pepsin, an enzyme focused on digesting proteins into amino acids, the “building blocks” of all our bodies proteins. When stomach acid is low, blood levels of essential amino acids are low. Stomach acid helps separate the minerals from the “food matrix” in which they’re found; when stomach acid is low, levels of many essential minerals are low.
Normally functioning stomach lining cells also make “intrinsic factor,” which should really be named after its function as “vitamin B12 absorption factor.” Without intrinsic factor, vitamin B12 can’t be absorbed, no matter how much we swallow! That’s why so many older people are taking/being given vitamin B12 injections, because their stomachs are sufficiently “gone” into “Gastropause” that they can’t help to absorb sufficient vitamin B12 from food or from supplements.
The effects of stomach acid reach beyond optimal digestion in the stomach. When food is fully acid-digested, the acid stimulates opening of the sphincter muscle separating the stomach from the duodenum (uppermost small intestine). When the acid and food are released into the duodenum, they stimulate the release of a hormone named “secretin,” which stimulates the pancreas to secrete bicarbonate.
Pancreatic bicarbonate not only neutralizes the gastric acidity, it also alkalinizes this part of the digestive process, which is necessary for maximal activity of the pancreatic enzymes to break down fats, carbohydrates, and the remaining undigested proteins into easily absorbable particles ready to be absorbed further down the intestinal tract. But without an adequate “secretin” signal released by optimal acidity and optimally digested food at the end of gastric digestion, the pancreas can’t do its digestive job optimally, either.
Optimal stomach acid is necessary for the best of health! How can we possibly expect to stay healthy if enough fully-digested nutrients are not available to keep these bodies within which we spend our lives on planet Earth as well-repaired as possible? It should be no surprise that the Mayo Clinic researchers found that after age 60, a larger percentage of individuals who had low stomach acid weren’t with us anymore! Stomach acid is literally tied to how long we live!
Other adverse health effects of “Gastropause” also happen. One is the growth of an increasingly “unfriendly” intestinal microbiome. An obvious example of this is acne rosacea, which results from the growth of bacteria in the upper small intestine that can’t grow there at all if the acid passing into it from the stomach is optimal. For details – along with citations – concerning curing (yes, that’s curing) acne rosacea with nothing more than hydrochloric acid supplementation, see the June 2017 Green Medicine Newsletter.
Many other unfriendly micro-organisms are also encouraged to grow in the more alkaline intestinal environment caused by “Gastropause.” One of the best examples of this is Candida Albicans, sometimes called “yeast infection,” which can live in the intestines with or (more often) without causing local intestinal symptoms. Candida in the bowels can cause health problems elsewhere in our bodies, including mental health problems.2
Another major problem caused by “Gastropause” is gastro-esophageal reflux. Despite the research published in 19693 that reported that stomach acid closes (not opens!) the sphincter muscle separating the stomach from the esophagus, patent medicine companies have raked in hundreds of billions of dollars selling the myth that “too much acid causes heartburn,” and using that research-disproven theory, simultaneously selling “acid blocking” medicine to “cure” the problem. Since most acid-blocking patent medications literally cause “Gastropause,” it is and was obvious that acid-blocking patent medications would increase dementia and a long list of other illnesses, all associated with the 100% “Gastropause” and very poor nourishment that these patent medicines cause.
The following article is updated from Chapter 1 of “Why Stomach Acid Is Good For You: Natural Cures for Heartburn and Indigestion” by Jonathan V. Wright, M.D., and Lane Lenard Ph.D. (2001).
The myth of acid indigestion
Heartburn, indigestion, dyspepsia, and “acid indigestion,” are extremely common afflictions. Thanks mostly to diet and lifestyle factors, and sometimes because of genetics, pregnancy, anatomy, or simple aging, it seems like sooner or later, almost everybody gets an upset stomach in one form or another. Who hasn’t felt the acute burning in the back of the throat and upper chest after eating certain foods? Who hasn’t popped a Tums or gulped a “bicarb” to extinguish the acidic flames that seem to roar up from the stomach during a heartburn attack?
A Gallup Poll found that 44% of the U.S. population suffers from heartburn at least once a month, and 7% experience it weekly. According to the National Institute of Diabetes and Digestive Diseases, 60 million people experience heartburn at least once a month and 25 million feel the burn every day.
If we are to believe what we see in the media, the American populace is awash in indigestion-causing stomach acid. We can’t watch TV (especially the evening newscasts) without seeing dozens of slick commercials for expensive, high-tech patent medicines like Prilosec,® Prevacid,® Tagamet,® Zantac,® Pepcid,® Axid,® and others, not to mention more traditional low-tech remedies like Tums,® Rolaids,® Maalox,® and Alka-Seltzer.® All of these products are designed to eliminate heartburn pain by reducing the amount of acid in the stomach.
The myth that underlies conventional “acid indigestion” treatment, and the implied message in all these commercials – although they never come right out and say it – is that heartburn happens because we’ve got too much acid in our stomachs. As a result, some of that acid flows back – or refluxes – into the esophagus, the muscular tube that carries food from the back of the mouth into the stomach. Since acid does not belong in the esophagus, its presence irritates the delicate tissue that lines the inside of the tube. Heartburn pain is basically a symptom of that irritation. If we’ve got heartburn or other symptoms of the more serious disorder, gastroesophageal reflux disease (GERD), the commercial message is clear: “The less acid we have in our stomachs, the better.”
We are also led to believe that if we simply have other feelings of indigestion, like “that overfull feeling,” with excess gas, bloating, or belching, but perhaps only a little heartburn, this is also due to “too much acid.” If this is true, then answer this question: Why is too much acid so inefficient at actually digesting food but so efficient at refluxing back into the esophagus?
To most “standard of care” physicians, it is “common knowledge” that heartburn and other symptoms of “acid indigestion” are signs of too much stomach acid. To relieve the pain, we need merely reduce the level of acid. If we believe this, it makes sense that we should all be using these powerful acid-reducing treatments to relieve our heartburn. According to the manufacturers of these products, long-term acid suppression is an advantage, allowing us to control heartburn “around the clock” perhaps with a single pill.
This kind of extreme heartburn protection may come at a cost to health that is being ignored by the pharmaceutical companies that patent and profit from these patent medicines, and also ignored by the Food and Drug Administration (FDA), which collected truly enormous sums of money to “approve” them. Most importantly the adverse effect on long-term health of these patent medicines is being ignored by the thousands of physicians who prescribe them. They fail to recognize that the acid-suppression theory, which currently governs the conventional medical therapy of “acid indigestion,” is seriously flawed. It is based on the myth that “acid indigestion,” heartburn, and its more serious consequence GERD are a result of too much stomach acid. The facts say otherwise.
Consider this conveniently overlooked observation: The incidence of indigestion, “simple” heartburn, and GERD increases with age, while stomach acid levels generally decline with age. If too much acid were causing these problems, teenagers should have frequent heartburn, while grandma and grandpa should have much less. Of course, as everyone knows, exactly the opposite is generally true.
It is simply a matter of common sense. How many of us can run faster at age 40 than at age 20? How many have better vision at 50 than when we were younger? We all experience declining hormone levels as we grow older. We can think of literally dozens of examples of naturally declining function with age, so why should the output of acid by the stomach be an exception?
Science has confirmed what common sense tells us. For most of this century, medical researchers have repeatedly and consistently documented an age-related decline in stomach acid. So, if we have less and less stomach acid as the years add up, why do we get more and more heartburn and indigestion? And more importantly, why are we treating that heartburn and indigestion by taking patent medicines that wring the last few drops of acid out of the stomach?
What’s so bad about depleting stomach acid? The list is a long one! Unfortunately, the conventional medical wisdom refuses to recognize this, which suits the makers of acid-depleting patent medicines just fine. The problem is that many of the adverse effects associated with long-term suppression of stomach acid may take years or even decades to develop, while clinical trials of most patent medicines, which might expose these problems, generally last only a few months.
Regrettably, many of the potential consequences of long-term acid suppression, including asthma, allergies, skin disorders, rheumatoid arthritis, insomnia, osteoporosis, gastrointestinal (GI) infection, depression, and many, many more can take years or even decades to develop. They would seem to have nothing to do with stomach acid, and therefore, would rarely if ever be reported.
GERD: The serious side of heartburn
It wasn’t too long ago that heartburn was viewed as largely a nuisance, something we joked about, put up with, blamed on Mother’s cooking. Today, heartburn is widely seen by the medical profession as the primary symptom of a potentially dangerous medical condition known as gastroesophageal reflux disease, or GERD. This shift in attitude has been driven in part by the availability (and marketing) of new patent medicines and surgical procedures and partly by new research. When heartburn occurs regularly for months or years, it is said to be chronic.
People with chronic heartburn may have damage to their esophageal lining (especially the lower end of the esophagus) that begins as mild irritation, but may end up with scarring, constriction, ulceration, and ultimately, in a very small percent of people, cancer.
This is why intermittent or minor heartburn should never be allowed to become chronic. Although GERD occurs only in a minority of people who have heartburn, given the potential danger of chronic heartburn, today’s acid-trumping treatments would seem to be among modern medicine’s more important, if under-appreciated, marvels. GERD appears to have met its match in these potent patent medicines that not only relieve heartburn but promise to protect us against more serious, even life-threatening conditions.
It’s no wonder they have become among the best-selling patent medicines ever produced. Indigestion / heartburn / GERD is a multibillion-dollar cash cow for the pharmaceutical industry. In the U.S. alone, we spent more than $7 billion on them in 1999. Prilosec® alone accounted for more than half of that, $4 billion, nearly doubling its sales from the previous year.
Indigestion and heartburn are not caused by too much stomach acid
As you might have guessed, we think there’s something dreadfully wrong with this rosy financial picture. We wonder why so much of humanity is going to such great lengths to rid themselves of all that annoying stomach acid, when very few of us have ever consistently had too much acid in our stomachs, ...when (except for a few rare conditions) heartburn is hardly ever associated with too much stomach acid.
Chronic heartburn sufferers often have their stomachs and esophaguses examined via x-rays and “gastroscopes” (fiber-optic tubes that allow the doctor to look inside the stomach and even take pictures), but in 30 years of medical practice, not one person who has had these procedures done elsewhere has ever told me that he or she has also had careful measurements made of stomach acid production! When we actually measure stomach acid output under careful, research-verified conditions, the overwhelming majority of heartburn sufferers are found to have too little stomach acid production.
Remember the research reviewed in the first part of this article? To repeat: the researchers reported that the lower esophageal sphincter muscle (for the technically inclined the “LES”) is closed in response to strong stomach acid. Think about that: it makes sense that if Nature and Creation have provided for humans very strong stomach acid for optimal digestion (pH 2 for the technically inclined; only vultures have a stronger stomach pH, reported4 to be 1.5) that there would also be provided (for those same humans) strong protection against that very strong acid digesting the lower esophagus too. That strong protection is provided by the lower esophageal sphincter, not by acid-blocking patent medicines!
Conventional treatments for heartburn and GERD
Acid Neutralizers (Antacids)
These classic products, commonly referred to as antacids, rely on the fundamental chemical fact of life that acid and alkali (also called “bases”) neutralize, or cancel each other out. The active ingredients are typically calcium, sodium, aluminum (not a good choice), or magnesium salts that combine with the normal stomach acid, hydrochloric acid (HCl), to form a “neutral” salt.
Since antacids do not affect the secretion of stomach acid, their effect on the gastric acidity is transient, lasting only until all the antacid molecules are used up. In the meantime, HCl continues to be secreted. Antacid products are easily available without a prescription and are widely regarded as extremely safe (except those containing aluminum). For occasional use, they can be useful for reducing heartburn and, when used this way, probably will not cause any harm.
Acid Blockers
Histamine H2-receptor blockers. These patent medicines (also called H2-blockers) reduce acid levels by throwing a roadblock right in the middle of the process that leads to acid secretion. Most gastric acid secretion is the end result of a process that begins with the hormone gastrin stimulating histamine-producing cells, which in turn signal acid-producing cells to secrete hydrochloric acid. By blocking the action of histamine, the message never gets to the acid-producing cells to secrete acid. These patent medicines can be very effective in turning off most of the acid flow for hours at a time.
The long-term, continuous suppression of gastric acid secretion has important adverse consequences for our health. These long-range adverse effects are noted above (repeatedly, sorry about that, but understanding them is important) and although very well documented by many researchers, they are largely ignored by practitioners of “standard of care” medicine. In addition, these acid-secretion-blocking patent medicines all have well-documented more rapidly occurring adverse effects, most of which involve GI disturbances, such as constipation, diarrhea, nausea, vomiting, and yes, heartburn.
Currently available H2-receptor blockers include Tagamet® (cimetidine), Zantac® (ranitidine), Pepcid® (famotidine), and, Axid® (nitazidine).
Proton Pump Inhibitors
The biochemical mechanism inside cells in the stomach’s lining that actually produce and secrete hydrochloric acid was named the “proton pump.” Proton pump inhibitors are the most potent of the acid-suppressing patent. They block the action of this pump mechanism, hence their name, proton pump inhibitors (PPIs). Just one of these pills is capable of reducing stomach acid secretion by 90% to 95% for the better part of a day.
Taking higher and/ or more frequent doses of PPIs, as is often recommended for “intractable” heartburn or for treating peptic ulcers, produces a state of achlorhydria (no stomach acid), duplicating the final phase of naturally occurring “Gastropause.”
There are many serious concerns associated with the use of PPIs. The most common short-term adverse effects include diarrhea, skin reactions, and headache, which can sometimes be severe. Other adverse effects, which occur less frequently, include impotence, breast enlargement, and gout. Currently available proton pump inhibitors include, Prilosec® (omeprazole), Prevacid® (lansoprazole), Aciphex® (rabeprazole), and Nexium® (esomeprazole).
But these patent medicines relieve symptoms
We’ve all heard of “short-term gain, long-term pain”? That’s what all of these “standard of care” treatments (given without ever actually measuring stomach acid) yield – short-term gain (unless you’re one of the many “lucky” ones who have relatively immediate adverse effects). None of these patent medicines cause the lower esophageal sphincter to close itself and block any acid reflux! They “work” by mopping up as much of the acid “flood” as possible (neutralizing antacids) or by drying up the river of acid itself (patent medicines such as Zantac® and Prilosec®). In so doing, they stop the heartburn pain while accelerating the aging process by causing malnutrition!
The relief anti-acid patent medicines offer is transient. Heartburn stays away only as long as acid levels stay suppressed, and acid levels stay suppressed only as long as we keep taking the patent medicines. If we stop taking them, we risk heartburn’s return, sometimes with a vengeance. We medical types like to call this a relapse. It’s not uncommon for people using Zantac,® Prilosec,® and even Tums® to take them daily for years and years at a time in order to avoid a relapse. Now that many of these patent medicines are available over-the-counter (without a prescription) and are promoted as being equivalent to (in terms of safety and ease of use, at least) and much more effective and longer-lasting than old-fashioned acid neutralizing products, people are even more likely to overuse them.
These patent medicines disrupt the natural gastrointestinal environment. Although widely believed to be safe and well-tolerated, acid-blocking patent medicines, by their very nature, induce profound changes in the internal environment of the stomach and intestines. These changes, which we will discuss in more detail in later chapters, have been associated with a wide range of ailments. Decades of research have demonstrated that chronically low levels of stomach acid (not necessarily caused by patent medicines) can be harmful in the long run, leading to maldigestion, malabsorption, and malnutrition.
We can become dependent on anti-acid patent medicines. Once we start taking anti-acid patent medicines, we may become dependent, or at least reliant on them. They work only as long as you keep taking them. Stopping treatment commonly triggers an acid “rebound,” which can be quenched only by – you guessed it – taking more acid-suppressing patent medicines. Although the rebound is typically short-lived, lasting a couple of days at most, how many people are willing to “tough it out” and endure the heartburn when they can quickly squelch it by getting back on their acid blocker? While this isn’t exactly a true addiction, once this cycle gets going, we’re almost as good as “hooked” on acid suppression.
This strategy works very well for patent medicine companies, but leaves much to be desired for people suffering from heartburn. If these patent medicines actually cured heartburn/GERD, the companies wouldn’t make nearly as much money as they do by selling patent medicines that provide only temporary relief.
A much safer “temporary fix” (but keep it temporary!)
Refluxin™ is a safe, effective, totally natural but very little known source of heartburn/acid reflux relief. Refluxin™ tablets (chewed and swallowed after meals) contain a combination of mucoprotective (protective of mucous membranes) natural agents, pectin, lecithin, and mucin which form a “floating raft” when in contact with liquid. A small amount of sodium and potassium bicarbonates reacting with citric acid provides buoyancy. When reflux occurs, the “floating raft” becomes part of the reflux, coating the lower esophagus with a safe natural barrier to acid penetration. But since the “Refluxin raft” literally floats on top of the food, it interferes much less with the digestive process.
Refluxin™ is indeed safe and effective to relieve heartburn, but should be used by heartburn sufferers only until thorough evaluation (and subsequent treatment) can be done by a physician skilled and knowledgeable in natural medicine. That’s because Refluxin™ treats the symptoms but not the cause of heartburn, which is usually – although not always – caused by lower (sometimes much lower) than optimal stomach acid.
It’s your decision
If you have indigestion or heartburn, a disease very frequently associated with low stomach acid output and poor digestion, which would be preferable: treat the cause or take a drug to suppress the indigestion and heartburn and then more patent medicines for each other symptom? The answer appears obvious, yet it’s going to be a long time before patent medicine companies give up their antacid / acid-blocker cash cow.
Fortunately, you don’t have to wait until the FDA, the AMA, and the many other alphabet-soup agencies that control the conventional wisdom in medicine today (almost always following the patent medicine industry line) see the “error of their ways.” (Hint: it’s never going to happen, because there’s so little profit in the natural – unpatentable – acid, vitamin, mineral, amino acid, herbal, and other supplements that can be used to eliminate heartburn, indigestion, and to treat related diseases.) You could go down to your local health food store right now and purchase everything you need for a fraction of the cost of a prescription for Prilosec,® Prevacid,® or other acid suppressor.
Before you do that, though, we suggest you read “Why Stomach Acid is Good For You” (from which this article is adapted) first, because you’ll learn:
- As we age, stomach acid levels do not increase, as we would expect from the increase in heartburn associated with age. In fact, for many people, acid levels decrease.
- Overuse of neutralizing or buffering antacids, and ordinary use of powerful acid-suppressing patent medicines, can inhibit the absorption of essential nutrients and impair the digestion of protein, minerals, and a few vitamins.
- The resulting malnutrition can, over many years, lead to depression, osteoporosis, arthritis, and other chronic degenerative diseases that reduce the quality of our lives and may ultimately shorten our lifespans.
- The best way to treat “acid indigestion” is not with less stomach acid, but (almost always) with more. Remember, optimal stomach acid itself “closes the door” between the stomach and the esophagus. Replacement acid in the form of safe, inexpensive substitutes for endogenous (internally-produced) stomach acid, such as betaine hydrochloride with pepsin, enhances digestion, and heartburn, indigestion, bloating and gas eventually vanish.
- The improved digestion and absorption of essential nutrients that results from appropriate acid replacement, combined with natural supplemental digestive enzymes and elimination of toxins and allergens, improves health and extends longer life, and improves the symptoms of a long list of diseases associated with low stomach production.
Sorry to be repetitive and possibly boring: the cause of heartburn and GERD is failure to close the lower esophageal sphincter muscle with strong acid, so “standard of care” treatment of heartburn and GERD with acid-blocking patent medications is actually malpractice!
While heartburn/acid indigestion is most frequently a symptom of “Gastropause,” other causes of these symptoms exist. Food allergy is one; some individuals report that heartburn and indigestion disappear when specific foods (often dairy and gluten, coffee, and alcohol) are eliminated. And while lower than optimal stomach acid/”Gastropause” often occurs because of “getting older,” another cause can be viral infection.5,6 Of course, the bacterium Helicobacter pylori is also a common cause of low stomach acid / ”Gastropause.”
Testing for “gastropause”: notes of caution
Please work with a practitioner skilled and knowledgeable in natural medicine who can very precisely measure whether or not you have less than optimal stomach acid (“Gastropause”) using equipment whose use is described as “gastric analysis by radio-telemetry” (also called “Heidelberg Capsule”) testing. Make sure – ask this physician’s office before doing any testing – that the procedure being followed in the use of this equipment is the one reported by researchers at the University of Toronto7 in 1970. (Yes, that’s 1970; it’s still the best testing protocol! If this equipment and protocol is not being used, please find another physician who uses them both!)
If less than optimal stomach acid is found by this testing and betaine hydrochloride is recommended, make sure the physician measures levels of nutrients (minerals with the hair mineral analysis, amino acids with the “fasting plasma essential amino acids” test) before and after taking betaine hydrochloride capsules for two or three months to be sure the number of betaine hydrochloride with pepsin capsules recommended to be taken with meals is sufficient to optimize levels of these nutrients.
As nearly all health food stores, compounding pharmacies, and the Tahoma Clinic Dispensary sell betaine hydrochloride with pepsin capsules, some of us decide to “skip the testing” and “just take the stuff” with meals to observe whether heartburn is relieved. Often it is, but (sorry about the repeat) the “before and after testing” noted in the last paragraph is the best way to determine if the number of capsules per meal (which can vary widely from person to person) is optimizing nutrient digestion.
Last caution: Some of us who “skip the testing” and “just take the capsules” suffer from increased heartburn! This does not mean the capsules aren’t needed! A “pain response” to betaine hydrochloride with pepsin often means that the stomach lining is so weak it “can’t handle” the added hydrochloric acid as it did for nearly all of us when we were teenagers!
An analogy for adults: before menopause, having consensual sex rarely causes women pain; after menopause, the exact same activity sometimes does hurt. The vaginal membranes have actually atrophied too much for those women. Fortunately, bio-identical hormone replacement almost always eliminates this problem, but that’s a “story for another time.”
Pain after taking betaine hydrochloride with pepsin is also often caused by a weak stomach lining, which can be significantly reversed by all-natural means, and betaine hydrochloride with pepsin not only doesn’t hurt anymore but does what it’s supposed to do to improve and ultimately optimize digestion once again. Unfortunately, acid production itself by the stomach lining cells rarely returns.
In conclusion (finally!)
Heartburn is usually a benign condition, but if you suffer from it regularly for months or even years at a time, it can be a sign of a serious disease, such as an esophageal ulcer or Barrett’s esophagus, a serious condition that can lead to a fatal form of cancer. Thus, we always suggest that the first step you take in treating your heartburn is to consult a physician who can rule out ulcer and Barrett’s and who will then guide and support you in treating your heartburn / GERD the natural way. The final chapter of “Why Stomach Acid Is Good For You” will tell you how to find a knowledgeable physician who, when you utter the words heartburn and indigestion, won’t automatically reach for the Prilosec.®
References
- VanZant F et al., “Normal Range of Gastric Acidity from Youth to Old Age,” Archives of Internal Medicine 1932;49(3):345
- For further information on “remote” effects of Candida Albicans, see “The Missing Diagnosis” by C. Orian Truss M.D., available at www.usedbooksearch.co.uk.
- Giles GR, Humphries C et al., “Effect of pH changes on the cardiac sphincter.” Gut 1969;10:852856
- Gremellit D, Prudor A, et al. “Vultures of the Seas: Hyperacidic Stomachs in Wandering Alabatrosses as an Adaptation to Dispersed Food Resources, including Fishery Wastes.” PLoS One 2012 June:7(6);e37834
- Gledhill T, Leicester RJ, et al. “Epidemic hypochlorhydria.” BMJ 1985 May;289:1383- 1386
- Ramsey EJ, Carey KV. “Epidemic gastritis with hypochlorhydria.” Gastroeneterology 1979;76:1449-57
- Andres MR, Bingham JR. “Tubeless gastric analysis with a radio-telemetering pill” (Heidelberg capsule). CMA Journal 1970;102:1087-1089. This article has been posted at the Green Medicine Newsletter website.
Reprinted with permission from Dr. Jonathan V. Wright’s newsletter, November 7, 2018. To subscribe: www.GreenMedicineNewsletter.com. All rights reserved. Please do not distribute.