PhotodynamicTherapy-NIHNCI-AV-8804-3748.jpg
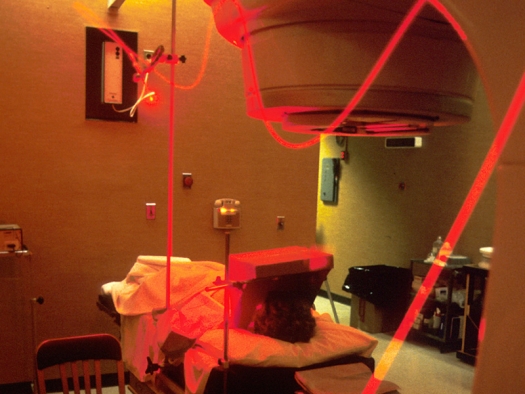
Photo by John Crawford / NIH: National Cancer Institute
Seen is a “beam of light” traveling along fiber optics for photodynamic therapy for use in an operating room. Its source is a laser beam which is split at two different stages to create the proper “therapeutic wavelength.”
The patient has been given a photo sensitive drug containing cancer killing substances which are absorbed by cancer cells. During the surgery, the light beam is positioned at the tumor site, which then activates the drug that kills the cancer cells, thus photodynamic therapy.
Summary
Objective: Introduction of a new treatment option in oncology: Photodynamic tumor therapy.
Method: Combined application of natural and chemically derived highly specific photosensitizers and new catheter-based laser technology for light activation of these photosensitizers to induce selective destruction of tumor tissue. Additional low-dose chemotherapy with light activation of chemotherapeutic drugs.
The combination with hyperbaric oxygenation is an option to optimize therapeutic results because oxygen radicals are responsible for tumor necrosis and apoptosis. Combination with immunotherapy like macrophage activating factor GcMAF can be of benefit as well.
Results: Different case reports indicate the great potential of the treatment regime.
Conclusion: Photodynamic tumor therapy and additional low-dose chemotherapy with light activation of chemotherapeutic drugs seems to be a promising new treatment regime in future oncology.
Introduction
Photodynamic therapy is one of the most interesting and promising approaches for treatment of various cancers. It has a long history and is already approved for some superficial cancers on the skin or on superficial layers in the esophagus or bronchial system.1,2,3,4,5 Treatments are easy to perform and – in contrast to chemotherapy – go normally along without severe side effects.
The principle is the stimulation of a light sensitive drug (photosensitizer) that is either applied on the skin as a cream or injected into the blood circulation. Through endocytosis the photosensitizer will be transported into the tumor cells anywhere in the body with high specificity. The process takes several hours (depending on the photosensitizer) and tumor cells will be light sensitive at the end.
Tumor tissue is subsequently irradiated with light of specific wavelength that matches the absorption spectra of the various photosensitizers to activate the latter. This light activation process induces various chemical processes such as the development of radical oxygen species that ultimately lead to the destruction of tumor tissue. Other than chemotherapy, photodynamic therapy thereby even stimulates the immune system in different ways.8,9
Until recently, PDT has been limited to treatment of superficial cancers as there was no technology available that would facilitate light application in deeper areas of the body. The relevance of that stems from the limited penetration depth of light in general and laser light of most wavelengths in particular: most of the light energy is absorbed by the skin and an effective light activation of photosensitizers that have accumulated at inner tumors was thus impossible in most of the cases. Due to this limitation, progress of PDT has been slow until today and consequently, the great challenge for application of this method for inner cancers is the delivery of light to into the body.10,11
Nowadays, new technological developments facilitate “systemic photodynamic therapies” and interstitial laser therapies and are thus able to overcome the “skin barrier.” They constitute the basis for extensive growth in this field.
Read the full article: Intravenous and Interstitial Photodynamic Laser Therapy, by Dr. Weber. Warning: This article includes graphic, revealing images of people receiving medical treatments that may not be suitable for all audiences.
References
- Allison, R.R., Sibata, C. H.: Photodynamic Therapy; Chapter 24. Perez and Brady’s Principles and Practice of Radiation Oncology, 5th Edition, 2008
- Allison, R.R., Sibata, C. H.: Oncologic photodynamic therapy photosensitizers: A clinical review. Photodiagnosis and Photodynamic Therapy 7, 61-75, 2010
- Bown et al.: Photodynamic therapy for cancer of the pancreas In: Gut 2002, April, 50(4):549-557
- Braathen, L. R., Hunger, R. E., Kernland Lang, K.: Photodynamische Therapie (PDT), Kap. 4.5. Tumoren der Haut, 2010, Georg Thieme Verlag KG
- Bruzell, E. Morisbak, H. Tønnesen, 2005 Studies on curcumin and curcuminoids. XXIX. Photoinduced cytotoxicity of curcumin in selected aqueous preparations. Photochemical & photobiological sciences. 4 7 (July), 523 530 , 0147-4905X
- Calin, M. A., Parasca, S. V.: Photodynamic therapy in oncology. Journal of Optoelectronics and advanced materials Vol. 8, No. 3, June 2006, p. 1173-1179
- Eichler, K., Engelmann, K., Mack, M. G., Straub, R., Vogl, T. J., Zangos, S.: Interstitielle Photodynamische Lasertherapie zur Behandlung von Lebermetastasen: Erste Ergebnisse einer in vivo Phase I-Studie. Fortschr Röntgenstr 2003; 175:682-687, Georg Thieme Verlag Stuttgart
- Eichler, K., Engelmann, K., Herzog, C., Mack, M. G., Thalhammer, A., Vogl, T. J., Zangos, S.: Interstitial photodynamic laser therapy in interventional oncology. Eur Radiol (2004) 14:1063–1073
- Jaeger et al.: A New Finite Element Approach for Near Real-Time Simulation of Light Propagation in Locally Advanced Head and Neck Tumors. In: American Journal for Neuroradiology (AJNR Am J Neuroradiol 26:1193–1200, May 2005.).
- Kaplan et al: Systemic Photodynamic Therapy in the Combined Therapy of Patients with Malignant Neoplasms with Metastases; Book of Abstracts, int. Laser conference Helsinki 2008
- Liu et al.: Hypericin and photodynamic therapy

