CoronaryArteryDisease.jpg
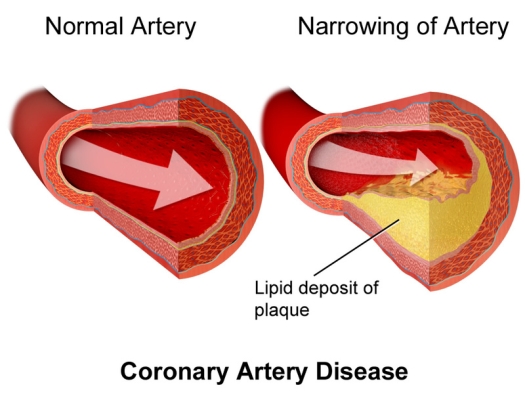
Illustration by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine.
Arterial plaque is the number one killer in the world – by far. If we can put a man on the moon, how come we can’t crack that code? Could it be that we are looking for causes in all the wrong places?
Here’s the story Pharma and friends have been feeding us for the last 40 years: The plaque in our arteries is caused by elevated LDL cholesterol levels. These plugged-up arteries are what cause strokes and heart attacks. So, the way to prevent strokes and heart attacks is obviously to lower LDL. And the best way to do that is to start eating drugs that lower LDL cholesterol. There is not one person in the entire U.S. that has not been indoctrinated with this story. But, what if it’s not true?
What if plaque is not caused by LDL? What if something else, something entirely unrelated to any form of cholesterol, is behind plaque buildup? In that case, does lowering LDL levels play any role at all in plaque formation? And, if LDL is not what is causing plaque, what is?
I’m pretty sure that you are going to be very surprised at the answer to these questions. So, hang on friend, it’s going to be a bumpy ride. It always is when everything you’ve been told is a lie! That is a very bold statement that I intend to back up.
According to WebMD, “Cholesterol plaques form by a process called atherosclerosis. Another name for atherosclerosis is the ‘hardening of the arteries.’ LDL or ‘bad cholesterol’ is the raw material of cholesterol plaques. Progressive and painless, atherosclerosis grows into cholesterol plaques silently and slowly. The eventual result is blocked arteries, which places blood flow at risk.”
So, there you have it. It’s that darned bad cholesterol that’s the culprit. It “silently and slowly” builds up in our plaques. So, for sure when the contents of plaques are analyzed they must be loaded with all that cholesterol. But, oops. That’s not what researchers find.
When plaques are analyzed, there is little-to-no cholesterol in them. Hard to believe? In 1991, the American Journal of Cardiology published an analysis of what is in plaque. Here it is: Fibrous tissue = 87±8%; calcium deposits = 7±6%; foam cells = 1±1%; and pultaceous debris = 5±4%. Pultaceous debris is defined in the medical dictionary as “pulpy.” In this analysis, these researchers found no cholesterol. A later study, this time by the American Heart Association, looked more closely at what was in a plaque.
In 1995, they found that the foam cells consisted of macrophages; the fibrous material consisted of fibrinogen, collagen, elastin, and smooth muscle cells; the calcium deposits obviously consisted of calcium, and the pulpy stuff was a mix of lymphocytes, lipids, lipoproteins, and proteoglycans. I don’t see cholesterol listed there, do you? Amazing! However, remember the presence of the fibrinogen and the lipoproteins, because I will be referring to them later.
To be honest, this does not prove that there is absolutely no cholesterol at all in plaques. It just shows that if there is any, it is very hard to find. And it certainly is not what causes plaque buildup. And here’s the point. What little cholesterol there may be in plaques cannot possibly come from LDL anyway. It must come from another source. That statement will need some explanation.
The little cholesterol that can be found in plaques is in the form of cholesterol crystals. Cholesterol crystals can only come from free cholesterol. Biochemically speaking, you can’t make cholesterol crystals when cholesterol is bound in a molecule referred to as an ester. And it might interest you to know that LDL cholesterol is just that – an ester. Therefore, the cholesterol crystals that can be found in plaque cannot come from LDL cholesterol. OK, then where do they come from? What is by far the most abundant source of cholesterol crystals in the body? It’s red blood cells. Remember that.
How about the lipoproteins in the plaque? Where do they come from? I was hoping you’d ask. LDL is a lipoprotein. So, is it possible that the lipoprotein in plaque comes from LDL? The answer is no, it’s impossible. Here’s the explanation. Stay with me because this can get a little messy.
LDL cholesterol contains two lipoproteins, LDL and another lipoprotein called apolipoprotein B. So, LDL cholesterol = LDL plus apolipoprotein B. There’s another lipoprotein called Lipoprotein A or Lp(a) for short. Lp(a) contains LDL and apolipoprotein B just like LDL cholesterol does, but Lp(a) also contains a third lipoprotein called apolipoprotein A. Think of it this way: LDL cholesterol = LDL plus apolipoprotein B. Lp(a) = LDL plus apolipoprotein B and apolipoprotein A. So, if you were to find LDL in plaque along with apolipoprotein B and apolipoprotein A, you know that it comes from Lp(a) not LDL cholesterol. Here’s why this is so critical.
In a study appearing in the journal Atherosclerosis, the researchers discovered exactly that. “Our studies imply that Lp(a) enters the arterial wall and accumulates extracellularly, where apolipoprotein B and apolipoprotein A can be co-localized with immunochemistry.” The underline is mine. The presence of both apolipoprotein A and apolipoprotein B indicates that the lipoproteins that were found in the American Heart Association analysis of arterial plaque came from Lp(a), not from bad old LDL cholesterol.
So, since LDL cholesterol is not in plaque and can’t possibly cause plaque accumulation, what does? Here’s where the plot thickens. Or should I say where the “clot” thickens? Because all the evidence that I am now going to report to you is pointing to abnormal clotting as the ultimate cause of arterial plaque, not LDL cholesterol. And if that’s what causes plaque, then all that money spent on reducing LDL cholesterol is missing the target. So, what is the evidence that clots are causing arterial plaque, how do they do it, and does LDL cholesterol have any role at all in the process?
The answer to those questions starts with understanding the endothelium. The endothelium is the inner lining of the arteries. Plaques form under the endothelium. But in order for the plaque to form under the endothelium, the endothelium has to be damaged. That’s where LDL cholesterol comes in. When it is oxidized, LDL cholesterol can damage the endothelium.
Oxidizing a molecule is what happens when an oxidant such as a free radical steals an electron from the molecule. When an oxidant steals an electron from LDL cholesterol it becomes oxidized LDL cholesterol or ox-LDL for short. Ox-LDL is able to damage the endothelium. LDL cholesterol that is not oxidized is harmless. And here’s the problem with all the drugs that lower LDL cholesterol.
Pharma doesn’t have a drug for ox-LDL. The drugs Pharma pushes do not distinguish between non-oxidized LDL and ox-LDL. They decrease all LDL. So, the only way Pharma docs know how to reduce ox-LDL is to reduce all LDL, oxidized and non-oxidized. But that approach is just not safe. And it is one of the reasons that the drugs are so harmful.
It’s not safe because every single cell in the body, especially nerve and brain cells, depends on an adequate amount of non-oxidized LDL. When that is decreased, things start falling apart. And all the problems that come with cholesterol-lowering drugs like cognitive decline, kidney failure, muscle pain, heart failure, and diabetes can take hold.
So, what causes the formation of the oxidants that oxidize LDL? It’s anything that can cause oxidant stress. Oxidant stress is universally accepted as the single most influential player in aging and age-related diseases, and high levels of ox-LDL are one reason why.
The primary cause of oxidant stress is decreased mitochondrial efficiency and/or a deficiency of antioxidant nutrients like vitamins C and E. I have reported before on how to reduce ox-LDL. It's simple. Just make sure you are in great cardiovascular shape, have good mitochondrial function as determined by Bio-Energy Testing (www.bioenergytesting.com), and have a diet high in antioxidants. The antioxidants that work especially well to reduce ox-LDL are pomegranate juice and vitamin E. But ox-LDL is not the only way that the endothelium can become damaged. So even if your levels are low, it doesn’t mean that you won’t develop plaque.
Other factors that can injure the endothelium are vitamin C deficiency, high blood pressure, elevated homocysteine levels, inflammation, diabetes, decreased nitric oxide, smoking, lead accumulation, NSAID drugs (such as ibuprofen, etc.), potassium deficiency, sodium deficiency, elevated blood sugar, and infections, particularly periodontitis. Remember these factors, because in order to avoid plaque and atherosclerosis, they need to be attended to.
But even if all of the above factors are absent, there is still some endothelial damage. It’s a normal consequence of life. But, not to worry. We have one system that heals the damage. It’s the clotting system. I’ll discuss that later. We also have another system that protects the endothelium from being damaged. So as long as these two systems are operating efficiently, everyday normal endothelial damage is not going to be a problem.
The system that prevents the endothelium from being damaged is the glycocalyx. The glycocalyx is a layer of proteins and sugars (glycoproteins) that line the endothelium. It is what makes fish so slippery. Because it is so slippery, the glycocalyx is able to protect the endothelium from injury. Additionally, it also contains various anti-coagulants to prevent clotting. Basically, without the glycocalyx, our endothelium would be constantly damaged, and the clotting that is designed to heal the damage would be uncontrolled.
Moreover, the glycocalyx blocks anything from getting past the endothelium and causing damage to the arteries. It’s yet another reason why cholesterol cannot cause plaque buildup – it can’t get past the endothelium. One review article stated that the glycocalyx “acts as a barrier against leakage of fluid, proteins, and lipids [like cholesterol and other fats] across the vascular wall.” To the degree that the glycocalyx is not functional, plaque will be the result.
I’ll talk about how to protect your glycocalyx later on. Now, let’s put all this information together in order to determine what really causes plaque and how to prevent it.
When the endothelium is damaged for any of the reasons mentioned above it causes bleeding into the inner layer of the artery. To counteract the bleeding, the body immediately sends platelets to the damaged area. The platelets release hundreds of chemicals and clotting factors, which act to draw in red blood cells, white blood cells, and Lp(a).
This collection of platelets, red and white blood cells, and Lp(a) forms a clot, which then acts to stop the bleeding and heal the endothelium. The chemicals also start converting fibrinogen into fibrin. Remember the fibrinogen part, because the more fibrinogen you have in your blood, the more fibrin you will form. The fibrin acts to tightly bind the clot together. And that is where the problem lies.
After the clot has done its thing by stopping the bleeding and stimulating healing, it is no longer needed and needs to be removed. To do that the body releases enzymes called fibrinolytics, which dissolve the fibrin in the clot and so eradicate the clot. The end result of the whole process is a completely healed endothelium. But many people have a problem when it comes to dissolving the clot. It has to do with the amount of Lp(a) in the clot.
People with high levels of Lp(a) have 3-4 times the risk of plaque than those with lower levels. That’s because the more Lp(a) you have in your blood, the more gets pulled into the clot when it is forming. That’s bad because Lp(a) blocks the formation of the clot-dissolving fibrinolytic enzymes. The result is a clot that never gets cleared and continues to build up in the arteries. Ultimately, it is these persistent clots that form the basis for plaque formation.
So by now, I’m betting you are wondering what proof there is that this is how plaque really forms. Here’s the proof:
One indicator is as I mentioned above, all plaques, while they contain very little cholesterol if any, do contain large amounts of fibrinogen. There is no way that fibrinogen can be in a plaque except as a result of the clotting process. Fibrinogen also acts to stimulate the production of the smooth muscle cells found in plaques.
Another indicator is the fact that plaques contain red and white blood cells. These cells are commonly found in clots. And, as I mentioned above, the red blood cells are the only possible source of the cholesterol crystals found in plaques. The white cells serve as the source of the foam cells that are found in plaques.
And here’s the point in all of this – there is no way the cholesterol theory can account for any of this. But don’t stop there.
Once a plaque has formed, it tends to rupture and cause more bleeding in the area. The same process that caused the plaque in the first place repeats itself again, leading to an even larger plaque. This is important because studies show that plaque does not develop slowly and steadily as is implied in the cholesterol theory. Plaque develops in phases. This explains how a patient can go from having a non-significant amount of plaque in a coronary artery that can suddenly and quickly enlarge to the point that he has a heart attack.
This kind of sudden plaque formation cannot be explained by the cholesterol theory but is typical for clot formation. According to the authors of one paper, “Subclinical [that means without any symptoms] episodes of plaque disruption followed by healing are a stimulus to plaque growth that occurs suddenly and is a major factor in causing high-grade coronary stenosis [blocked arteries].”
Perhaps the best single statement made by any researcher regarding what causes plaque comes from Elspeth Smith in her paper published in Thrombosis Research and titled “Fibrin as a factor in atherogenesis.” She stated, “After many years of neglect, the role of thrombosis [another word for a clot] in myocardial infarction is being reassessed. It is increasingly clear that all aspects of the hemostatic [blood clotting] system are involved: not only the acute occlusive event but also in all stages of atherosclerotic plaque development from the initiation of the atherogenesis to the expansion and growth of large plaques.”
Stated in non-medicalese, Smith is saying that it is “clear” that clot formation is what starts the initial formation of a plaque, is what causes plaques to continue to enlarge, and is what causes sudden heart attacks.
So, what is the major implication of all this evidence? It is simple. If you are trying to decrease plaque formation by lowering LDL cholesterol, you are wasting your time. What you need to do is to act on what really causes plaques: clotting. And next, I’ll show you how you can do that.
“You’ve Been Lied to About LDL Cholesterol and Heart Attacks!” was originally published in Dr. Frank Shallenberger’s Second Opinion newsletter, April 2023. Used with permission.