StaphylococcusAureusBiofilm-7486.jpg
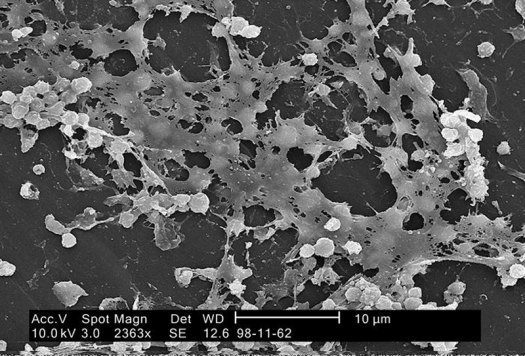
Photo ID#:7486 by Janice Carr, 2005 / CDC Public Health Image Library (PHIL)
Under a magnification of 2363X, this scanning electron microscopic (SEM) image depicted numbers of Staphylococcus aureus bacteria, which were found on the luminal surface of an indwelling catheter.
Of importance is the sticky-looking substance woven between the round cocci bacteria, which was composed of polysaccharides, and is known as “biofilm.” This biofilm has been found to protect the bacteria that secrete the substance from attacks by antimicrobial agents such as antibiotics.
Margaret, a long-time subscriber, had unsuccessfully battled an overgrowth of Candida albicans for over 10 years. She was desperate for help. Her Candida began as vaginal yeast that progressed to a chronic systemic fungal infection. It caused exhaustion, brain fog, bloating, diarrhea, and a host of other uncomfortable symptoms.
What’s more, it suppressed her immune system. This led to a number of other complications. For instance, she seemed to catch every cold and flu bug that came around. Before she could regain her health, she needed to get her Candida under control.
At first, Margaret stopped eating sugar – Candida's favorite food. When that wasn’t enough, she resorted to everything she could think of: more restrictive dietary changes, supplements to support her immune system, antifungal herbs and essential oils, and, finally, antifungal medications her doctor prescribed. Nothing worked for long.
Margaret wanted her life back.
After speaking with her, I believed I knew what was going on. I was convinced that she had a little-known condition found in up to 60% of chronic infections. It’s caused by an overgrowth of pathogenic bacteria and fungi. I believed that with the right treatment, Margaret could recover. She did.
If you suffer from a chronic infection, this issue will give hope that you can recover, too. Here’s how:
There is a little-known three-part therapy that stops many chronic illnesses in their track. A growing number of doctors also have found it works. As you know, I like to see the science behind a treatment before I write about it.
Unfortunately, there aren’t any studies on this therapy yet. But I’m hearing from so many women with chronic infections, that I wanted to get you this information now, not later. Until there are clinical studies, we can look at the evidence from these doctors’ observational studies, along with the research from a medical doctor who has developed this program.
So far there has been an exceptional response in people with a fungal overgrowth like Candida albicans and bacterial problems like H. pylori. There have also been excellent results in treating a number of other pathogens throughout the digestive tract.
If you have irritable bowel syndrome (IBS), urinary tract infections, Candida, or digestive problems (including ulcers), and you can’t get better no matter what you do, this may be why.
What’s more, if you’ve found no lasting resolution to your Lyme disease, periodontal disease, cystitis, or esophagitis, don’t give up. In fact, if you have any chronic bacterial or fungal condition that hasn’t responded to other therapies, help could be three steps away.
Antibiotics make it worse
When infections become chronic, a war rages in your body. And the pathogenic bacteria and fungi are winning. Antibiotics and antifungals may alleviate some symptoms initially, but they don’t address the source of the problem. In fact, it turns out that antibiotics actually make these pathogens stronger!
This is why some people never get well. The bacteria and fungi that are keeping them sick are successfully able to survive no matter which antibiotics, antifungals, herbs, and other substances they use.
Here’s what’s going on: Free-floating pathogenic bacteria come together to form a sticky substance, which encases them within a protective matrix. This prevents anti-inflammatory cells and antibiotics from reaching them. This substance is called biofilm.
The fascinating world of biofilm
You’ve heard about biofilm before, but maybe not by this name. In fact, you have it in your mouth and fight it every day. You know it as dental plaque. And it causes chronic infections from dental implants. This is why dentists are years ahead of medical doctors when it comes to understanding and treating oral biofilm. One of their treatments, ozone therapy, is very effective in treating oral biofilms. But it’s not as effective against those biofilms that live in the intestines where they’re more protected.
The eradication of biofilm in the gut is being investigated and researched by Stephen Olmstead, MD.
Most doctors, even doctors who practice integrative medicine, haven’t even heard about biofilm or its solution.
Biofilms are substances, common in nature, that form when free-floating pathogenic microbes join together and stick to surfaces. They can be the slime you find coating rocks in a stream, the “gunk” in your drains, or dental plaque. Or they can live hidden in your digestive tract or genitals where they can impair your health.
Biofilms are complex communities of microbes living within impenetrable protective “cages” made from various sugars, minerals, and other substances. These shells keep antibiotics and antifungals from reaching and destroying biofilms’ pathogens.
These masses of microbes are tenacious. They stick to surfaces like the metals and plastics used in medical devices. They also stick to the intestinal lining, where they contribute to numerous chronic illnesses. Some people with invasive candidiasis have fungal biofilms from dental implants, catheters, and heart valves.
If your health has deteriorated after a medical or dental procedure and antibiotics haven’t worked, you may have an excess of pathogenic biofilm. If this is the case, you may not be able to get well until you get these biofilms under control.
Biofilms are innately more resistant to antibiotics than free-floating bacteria. How resistant? They can be from 10 to 1,000 times more resistant to antibiotics than free-floating bacteria! At best, antibiotics may work initially. But a relapse is sure to follow. Similarly, Candida is resistant to common antifungals like fluconazole.
Finding a program that works
Each type of biofilm responds to a slightly different protocol so an individualized approach is essential. Dr. Olmstead advises doctors on the best protocol for each patient. He has been collecting clinical reports on treatments to eradicate biofilm. This is no simple matter, because fungal biofilm need a different protocol than bacterial biofilm.
Here’s what you need to treat biofilm:
First, you have to disrupt the protective shell surrounding biofilm that prevents antibiotics and antifungals from killing the bugs.
Next, you need to use the right antimicrobials to destroy the particular microbes inside your biofilm. These may be antibiotics or herbs, depending on which bacteria or fungi you need to eradicate.
Finally, you need to add pre-and probiotics to increase colonies of friendly bacteria. These bacteria strengthen your immune system so it can better fight infection from pathogenic biofilm.
While I wish it was possible for you to follow this program on your own, this is one case where a doctor is a necessity for getting a key ingredient in the antibiofilm protocol. You’ll need to find someone who’s willing to work with you to get your biofilm colonies under control.
Step #1: The biofilm solution
Biofilms are a major factor in antibiotic resistance in part because they live in a protective environment. So the first step is to break down the biofilm’s protective cage. It’s very much like a fortified city. To break it down, you need to use a combination of specific digestive enzymes, chelating agents, and natural antimicrobials. They disrupt the substances that form biofilm. Once you have compromised the biofilm, you need other nutrients to repair the intestines that the pathogens damaged.
The pathogenic bacteria in biofilm weave a protective matrix out of polysaccharides and proteins. These substances then attract metals and nucleic acids. So the first step is to damage this matrix, making penetration possible. Unless and until you do, there’s simply no way any antibiotic or other antimicrobials can destroy the pathogens within the biofilm.
What can break down this matrix? Enzymes.
Don’t think that you can pick up any enzyme or enzyme formula at your local health food store and start feeling better. Even if it’s strong. You need specific enzymes that are effective in binding to the cellulose in biofilm’s matrix, and others to attach themselves to minerals and protein. It takes the right enzymes in the correct potency taken over the right length of time to get results.
Dr. Stephen Olmstead, an MD at Klaire Labs, has researched biofilms for nearly a decade. He’s developed a combination enzyme formula that penetrates biofilms’ matrix, allowing antimicrobials to then kill off pathogens like H. pylori, Klebsiella, C.difficile, Candida albicans, MRSA, and others. It’s called InterFase™ and InterFase Plus™.
Begin with InterFase
Pathogenic biofilms can hide anywhere, from the sinuses to the large intestines. InterFase is a combination of eight enzymes specifically chosen for their ability to break down biofilms throughout the gastrointestinal (GI) tract. In addition, this formula also is available with Disodium EDTA. Both formulas are effective in disrupting biofilm made by various pathogens.
Calcium, magnesium, and iron are minerals essential to our health. They’re also essential to the formation of biofilm. Disodium EDTA binds to calcium and magnesium in the biofilm matrix, making them more permeable. Lactoferrin effectively binds to iron. But you should avoid it if you have a dairy sensitivity. Please don’t experiment with EDTA. It is best to use this chelating agent under medical supervision.
Step #2: Antibiotics and antimicrobials
Penetrating pathogenic biofilm isn’t enough. You also need to stop biofilm from multiplying, and you need to destroy some of the existing pathogenic biofilm. This is when and where antibiotics, antifungals, and antimicrobials come in. They may be anything from antibiotics to natural antimicrobials, such as the berberine found in golden seal root, oregano, and green tea extract.
But you’ll need to take enough of the right herb – or antibiotic – long enough to destroy biofilms’ pathogens. This means working with a knowledgeable health care practitioner to make sure you’re taking the antimicrobials that can best fight your particular bacteria or fungi. If he or she doesn’t know how to design a protocol for you, I’ll tell you shortly how to find someone who can.
Step #3: Re-establishing your gut health
Various probiotics (friendly bacteria) help reduce colonies of pathogens within biofilm in the GI tract. Not all probiotics are effective against all pathogenic bacteria. Prebiotics, which are foods for healthful probiotics, stimulate the growth of some of these beneficial bacteria. It’s vital to increase the good bacteria while decreasing the bad guys.
The prebiotics and probiotics you take to help reduce biofilm need to be the specific ones known to work with your particular pathogens. Your doctor can get some of this information in an article Dr. Olmstead wrote in the Townsend Letter (October 2009) and from Dr. Olmstead, at Klaire Labs.
Your next step
So, what should you do if you suspect your health problem is complicated by an overgrowth of pathogenic biofilm, knowing that your doctor probably hasn’t even heard about this problem? Different pathogens and the composition of their matrixes need different and specific, protocols. This is where Dr. Olmstead comes in.
Disrupting biofilm is simple, but tricky, especially since there are no tests to accurately determine the presence of pathogenic biofilm overgrowth. However, symptoms often disappear with this three-step antibiofilm program. The good news is that Dr. Olmstead is available to speak with your doctor and help design a protocol specifically for you. There is no charge from Dr. Olmstead for his services.
You need to take all of the supplements in this three-step program concurrently for at least two weeks. Some may need to take them as long as three months, or longer. You’ll need someone knowledgeable to help you understand what to take and for how long. You can obtain the InterFase enzymes and probiotics appropriate to your condition from your doctor through Klaire Labs. The ones you need to take depend on the type of pathogens you have.
Show this article to your doctor and ask him or her to call Dr. Olmstead at Klaire Labs (888- 488-2488) for further information.
The enzymes you need to take and how often
I know that this is a more complicated program than those I usually give you. But just think. It could be the solution to your chronic GI problems that haven’t yet been corrected with other methods.
References
Braz J Infect Dis. 2008 December;12(6):526-30.
Darvish, Dr. Nooshin K. “The Antibiotic Complicated,” 28/02/09.
Petrova, Olga E., and Karin Sauer. “A Novel Signaling Network Essential for Regulating Pseudomonas aeruginosa Biofilm Development.” PLoS Pathogens, 2009; 5 (11): e1000668 DOI: 10.1371/journal.ppat.1000668.
Originally published in Dr. Janet Zand’s Women’s Health Letter. Used with permission.


