SystemicLupusErythematosusSymptoms.jpg
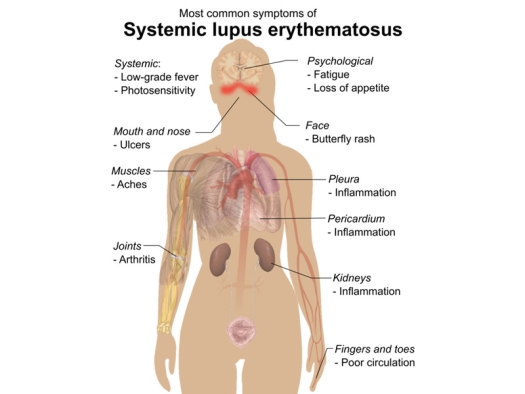
Illustration by Mikael Häggström (2014). "Medical gallery of Mikael Häggström 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.008. ISSN 2002-4436 via Wikimedia Commons / Public Domain
Part 1: Introduction
Lupus Erythematosus and Scleroderma are classified as vascular diseases, along with polyarteritis nodosa, and some other diseases, but Lupus and Scleroderma also have one other thing in common – they can be treated in a similar manner with equally good results!
Lupus Erythematosus is a chronic, nontuberculous disease of the skin marked by disklike patches with raised reddish edges and depressed centers, and covered with scales or crusts. These fall off, leaving dull-white scars.
Scleroderma is a disease of the skin in which thickened, hard, ridged, and pigmented patches occur. During the course of the disease, the connective tissue of the skin layer beneath the epidermis (corium) and the subcutaneous structures are increased and a "hidebound" condition results.
The ordinary form of Scleroderma begins in middle life, and is often considered, by traditional medicine, as incurable.
According to Richard A. Kunin, M.D., "Systemic Lupus Erythematosus is the classic example of immune system turning against specific cells in the body in joints. The immune complexes formed when antigen from cells combines with antibodies from immune cells, circulate until the spleen and kidney can excrete them. Along the way these may deposit in various tissues, causing secondary inflammatory disorders, such as nodules and inflammation of the skin and kidneys. The spleen is hard-pressed to digest and excrete all of these complexes and the overload can deposit in the kidney, causing great damage. In fact, this overload is the most serious complication of Lupus and a frequent cause of death."10
The Case of Suzie White
Suzie White, 40 years-of-age, had a 2 to 3 year history of finger stiffness and pain and swelling (edema) of toes and the fingers. She also had marked sensitivity to the sun, with mild to moderate butterfly lesions across her nose and cheeks. The Houston Medical Center (Texas) diagnosed Suzie's condition as Systemic Lupus Erythematosus. She was advised by that center to take gold shots, and the other traditional palliative and damaging treatments.
Instead, under the care of Ronald M. Davis, M.D.,20 Suzie decided to try intravenous EDTA (ethylene diamine tetracetic) chelation therapy and DMSO (Dimethylsulfoxide). These infusions also included magnesium sulphate, sodium bicarbonate, Vitamin C, pyridoxine, B-complex, dexpanthenol, and Vitamin B12.
Oral metronidazole and allopurinol – following The Arthritis Trust of America/The Rheumatoid Disease Foundation treatment protocol as described in "The Roger Wyburn-Mason, M.D., Ph.D. Treatment for Rheumatoid Disease."
She was very lax about taking her intravenous infusions and would come in weekly until she began feeling better, and then she'd wait 2-10 weeks before coming in again. Despite this laxness, Suzie did very well and became free of symptoms.
One year and eight months after starting her treatments with Dr. Davis, Suzie was given 2 hydrogen peroxide intravenous infusions (0.03%) within 2 hours of one another. She has been free of symptoms for the past 3 years.
Dr. Davis says, "As you can see, the anti-amoebic regimen is included in my treatment protocol. I believe this to be most important in treating these diseases. It is amazing how these patients respond to "The Roger Wyburn-Mason, M.D., Ph.D. Treatment for Rheumatoid Disease."
What is Systemic Lupus Erythematosus?
Systemic Lupus Erythematosus is an inflammatory connective tissue disorder of unknown cause occurring chiefly in young women, and also in children and older adults. According to Alan Gaby, M.D., the word "lupus" is latin for "wolf," and erythematosus means "redness," together the terms represent or refer to the red lesions appearing on the face and that resemble a wolf's bite.17
Historical Identification
Kaposi first recognized skin and visceral involvements in 1872; Osler described skin lesions (polymorphic) in conjunction with arthritis and kidney failure by the early 1900s. In 1920-30 Systemic Lupus Erythematosus was identified as a distinct disease. It is now recognized as a disease entity that evolved from a group of clinical manifestations that include characteristic pathological and laboratory findings.
Historically there have been two definitions: Cutaneous Systemic Lupus Erythematosus, and Systemic Lupus Erythematosus. This distinction is no longer felt to reflect two different diseases.
Distribution of Systemic Lupus Erythematosus
There may be as high as 1 per 100,000 among family members of those afflicted.
The prevalence among African-American, American-Indian and several Asian groups is higher than among Whites. Black females have a higher incidence rate of 7 to 8 per 100,000, as compared to 2 to 3 per 100,000 among White females.
The ratio of female-to-male is approximately 10 to 1, although this ratio is less likely in childhood when the disease occurs prior to puberty.
Both pre-puberty and postmenopausal groups reflect a ratio of 2:1 to 3:1.
Clinical Symptoms
Anemia; fever; hair loss; headaches; high blood pressure; inflammation of lung lining; inflammation of membrane surrounding heart; joint pain; kidney problems; sensitivity to light; skin lesions, including characteristic "butterfly" redness of skin over cheeks and bridge of nose; symptoms vary according to organ affected. Systemic Lupus Erythematosus manifests itself through body fluids (humoral) and cellular abnormalities and through tissue destruction in many different organs.
As this disease progresses, the afflicted may find that it has been diagnosed differently over time.
It may also be defined as a Mixed Connective Tissue Disease involving arthralgias or arthritis, swollen hands, inflammation of muscles (myositis), capillary congestion and swelling (Raynaud's phenomenon), gastrointestinal problems (esophageal hypomotility) and lymph system (lymphodenopathy). These characteristics are also accompanied by certain positive laboratory findings (high titers of antibodies to ribonucleoprotein).
As these characteristic symptoms often overlap in Systemic Lupus Erythematosus, the term "Mixed Connective Tissue Disease," drops out, and the terms "Systemic Lupus Erythematosus," or "Progressive Systemic Sclerosis," are applied more frequently.
Diagnosis Criteria
Because there are so many clinical manifestations and expressions of this disease, diagnoses can often challenge the clinician. No single finding or test result will confirm the presence or absence of this disease, but rather, accurate diagnosis lies with comparison against a pre-established set of criteria, as defined by the American Rheumatism Association.1 Any four or more of the eleven criteria presented, either in succession, or simultaneously, constitutes the basis for positive diagnosis.
Eight of these criteria include a history and physical examination which includes cheek rash, disc-like rashes, photosensitivity, oral ulcers, arthritis, inflammation of lung or heart membranes, kidney involvement, and nerve involvement with seizures or psychosis.
Two more criteria involve routine laboratory analysis supplying further evidence of involvement of various organs, as well as a complete blood count to identify various blood disorders.
One criteria requires more sophisticated laboratory tests, for antinuclear antibodies.
Other tests may be used to screen out additional diseases, such as for syphilis.
Onset of Systemic Lupus Erythematosus
Systemic Lupus Erythematosus may begin abruptly with fever, simulating acute infection, or can develop insidiously over many months or even years, with only occasional flare-ups of fever and discomfort.
Any organ that has been affected may also present with symptoms unique or characteristic to that organ.
As many as 90% of the patients complain of joint symptoms that range from intermittent to acute, single joints to many joints, some for months or even years before other manifestations occur.
The characteristic "butterfly lesion," or "erythema," is one of several skin appearances. Others include disc-shaped lesions, and other forms on the face, exposed areas of the neck, upper chest and back and other areas exposed to light. These lesions may join one another, making the skin worse in appearance (edematous).
Ulcers may appear in the central portion of the hard palate near the junction of the hard and soft palate, the cheek and gum mucosa and the anterior nasal passage. Blistering and ulceration are otherwise rare.
During active phases of the disease, loss of hair may occur.
Redness, swelling and reddish-purple lesions may show around the sides of the palms with extension of fingers, around the nails, and at the palms of the fingers.
Small blood vessels or the lymph system may be affected by inflammation, resulting in purple patches on the skin.
Sensitivity to light occurs with about 40% of the patients.
After long-standing disease, joint deformity, without joint erosion, is common, particularly deviation of the fingers and dislocation of certain finger joints (proximal interphalangeal).
Inflammation of the lining of the lungs may occur recurrently.
Bacterial or viral pneumonia is common.
Inflammation of the lining of the heart is often present. Heart problems, usually found after autopsy, have occurred in as many as a third of the cases.
A generalized glandular problem will occur particularly in children, young adults and Black people. Enlargement of the spleen occurs in 10% of the patients.
Involvement of the central nervous system causes personality changes such as epilepsy, pyschoses, and organic brain syndrome.
Kidney involvement occurs in the majority of patients, and may progress to a fatal end. Sometimes kidney dialysis is the only way to keep a patient alive.
Survival Outcome
The outcome of this disease depends mostly upon which organs of the body are affected, and how deeply. Patients with localized skin symptoms usually have a significant chance of long survival, while patients with kidney and brain involvement may have intermittent relapses, and still others may have prolonged remissions. Although the survival rate is mixed, according to the above-described organ deficiency situations, the survival rate is about 70%, with infection and kidney failure being leading causes of death.
Genetic Marker
Identical twins have a higher incidence of Systemic Lupus Erythematosus than do non-identical twins.
There appears to be a multi-gene influence on those with the disease. Those with a deficiency of certain substances in the blood (complement) and certain gene markers (HLA-DR2, HLA-DR3, HLA-B8, others) seem to have a higher incidence of the disease.
Other Causations
As with the other 80 or so Rheumatoid Diseases, Systemic Lupus Erythematosus may be considered to have multiple causes and probably should be treated in various ways, including proper nutrtional support.
Alan Gaby, M.D. reports on Nurses' Health Study that appears to show a strong relationship between Systemic Lupus Erythematosus and the use of estrogen therapy, suggesting that, at least in part, it is hormone-dependent.
Beginning in 1976, 69,435 postmenopausal nurses were followed for 14 years. To shore up the hormone-dependency link, Gaby explains that "First, the incidence of Systemic Lupus Erythematosus in adults is 8 times greater for women than for men. Second, Systemic Lupus Erythematosus patients of both sexes have abnormalities of estrogen metabolism. Third, women with Systemic Lupus Erythematosus have low plasma androgen (sex hormone) levels.
"It should be pointed out," Gaby says, "that most estrogen prescriptions are for horse estrogen (Premarin), which differs substantially from the homones secreted by the human ovary."11
According to A.V. Costantini, M.D.,14 a list of diseases wherein fungal forms of microorganisms have been found include the following: atherosclerosis, cancer, AIDS, diabetes mellitus, Rheumatoid Arthritis, Sjogren's syndrome, Systemic Lupus Erythematosus, Gout, Crohn's disease, multiple sclerosis, hyperactivity syndrome, infertility, psoriasis, cirrhosis, Alzheimer's disease, Scleroderma (Progressive Systemic Sclerosis), Raynaud's disease, sarcoidosis, kidney stones, amyloidosis, vasculitis, and Cushing's Disease.
Dr. Costantini, believes that the concept of "auto-immune" diseases contains a fatal flaw, because no successful species can develop a system of defense which attacks itself.
Antibodies that are measured in the blood stream and which imply an autoimmune condition are actually antibodies against "ubiquitin," a substance that is present in many species including that of fungi.
Traditional Treatments
Treatment must be individualized depending upon the location of problems or the severity of them. For purposes of treatment, the disease is classified as "mild" or "severe."
Mild disease is characterized by fever, arthritis, inflammation of the lining of the lungs or heart, and rashes.
Severe life-threatening disease involves anemia, massive heart and lung involvement, significant kidney damage, acute inflammation of the vascular system in the extremeties or gastrointestinal tract, Central Nervous System disorders and formation of purple patches on the skin and mucous membranes (thrombocytopenic purpura).
Mild Disease
Analgesics and Non-Steroidal Anti-Inflammatories
Salicylates (aspirin) are used to control the pain and fever.
Other non-steroidal anti-inflammatory drugs are also used, such as indomethacin or ibuprofen. Ibuprofen can be given for those who do not tolerate aspirin.
Anti-malarials
Anti-malarials, such as hydroxychloroquine or cloroquine, may also be used to control rashes or mucous membrane lesions.
Cortisone
Cortisone, taken orally in the form of prednisone, may be added to the regimen to control the symptoms of arthritis and muscle pain (polymyalgia).
Phenylbutazone
Sometimes phenylbutazone is alternated with the aspirin.
Severe Disease
Corticosteroid Therapy
Immediate corticosteroid therapy, usually in the form of oral predisone, is administered, which becomes the mainstay of the treatment.
The other analgesic and anti-inflammatory drugs are not used, because they have become, or are, ineffective.
In Both Mild and Severe Disease
After symptomatic inflammation is under control, minimal dosages of cortisone are used. Usually the dosage is decreased little by little.
Response to therapy is determined by relief of symptoms and signs, or improvement in other laboratory tests.
Infections are treated vigorously, usually with some form of antibiotic.
The usual measures for combating heart failure and kidney problems are employed, including kidney dialysis, if necessary.
Close medical supervision is extremely important during surgical procedures and pregnancy.
There must be concerted effort to eliminate emotional stress, physical fatigue, any implicated or unnecessary drugs, and excessive sunlight exposure.
What's Wrong With Traditional Treatments?
As is true for other rheumatoid diseases, traditional treatments primarily address symptoms and not their causes, and many of the traditional treatments have adverse side-effects.
Most important of all critical comments, there is no attempt to step outside traditional regimens that are doomed in advance to failure, insofar as bringing about health remissions or cures.
Mild Disease
Analgesics and Non-Steroidal Anti-Inflammatories
Aspirin and non-steroidal anti-inflammatory Drugs (NSAIDS) are useful for temporarily alleviating symptoms but do not address the causation of Systemic Lupus Erythematosus. Their extended usage, however, can result in several serious problems.
Salicylates, for example, can erode the lining of the stomach, leading to bleeding ulcers and other gastrointestinal problems. Enteric coated and buffered aspirin is of little use except for those who have peptic ulcers or hiatus hernia.
Sustained-release tablets might provide longer relief for some patients, and may help an individual through some intolerable pains.
Indomethacin has both analgesic and anti-inflammatory properties, and, unlike corticosteroids, has no effect on pituitary or adrenal glands.
Adverse effects of the usage of indomethacin are headache, dizziness, lightheadedness and gastrointestinal disturbances such as nausea, loss of appetite, vomiting, epigastric distress, abdominal pain and diarrhea.5 Gastrointestinal bleeding may also result from its use.
Indomethacin should not be given to a patient with active peptic ulcer, gastritic, or ulcerative colitis, conditions which can easily accompany a number of Rheumatoid Diseases.
Occasionally fluid retention is a problem.
Central Nervous System effects may be transient and disappear altogether on continued usage with dose reduction, but occasionally they are of such severe nature that therapy must be discontinued altogether.
Patients who show signs of Central Nervous System symptoms should not operate automobiles or other hazardous equipment.
Other nonsteroidal anti-inflammatory drugs such as ibuprofen can be given for those who do not tolerate aspirin. Although less of a gastrointestinal irritant than aspirin, it can produce gastric symptoms and gastrointestinal bleeding.
As the major share of pharmaceutical drug research – which is also the dominant share of arthritis research –is aimed at relieving symptoms for arthritics – not in achieving cures – there are always new analgesic, non-steroidal anti-inflammatory drugs being huxtered as "break-throughs." None of these help our bodies to heal.
Anti-malarials
As with phenylbutazone, hydrooxychloroqiune should be taken under close medical supervision as it may create irreversible retinal degeneration. With its usage, repeated eye tests are required by an opthalmologist before and every 2 to 3 months during treatment.5
There are also other serious effects involving the Central Nervous System, neuromuscular reactions, skin, blood, and gastrointestinal effects.
Cortisone
Although relief is nearly instant, on use of "cortisone," it doesn't halt the progression of the disease. Cortisone (prednisone) merely suppresses the symptoms or "clinical manifestations," acting at the microscopic level. It inhibits the early phenomena of the inflammatory process which includes swelling, blood clotting, capillary expansion, and capillary proliferation, fibroblast proliferation, deposition of collagen tissue and later scar tissue formation, and migration of white blood cells into the inflamed area and phagocytic activity.
All of the described functions which are inhibited by the use of cortisone are required by the human body for growth and repair of tissue.
Cortisone impairs wound healing and provides the grounds for predisposition to infection. It has major effects on the monocyte/macrophage systems, preventing the release of a substance that aids in fighting infection, Interleukin I.
Phenylbutazone
Phenylbutazone cannot be considered a simple analgesic, but should be used under careful medical supervision. It's usage can result in serious side affects of anemia and loss of certain leukocytes (agranulocytosis). Through it's use, there is an incidence of
2.2 deaths per 100,000 exposures from the above named conditions. The risk increases with age and long-term usage, especially women, to 6.5 deaths per 100,0005.
Other side effects include gastrointestinal, skin, heart, kidney and other serious effects.
Phenylbutazone has an anti-inflammatory effect but it also has severe toxic effects, including peptic ulcer, sodium and water retention, inflammation of the skin (dermatitis), inflammation of the mouth (stomatitis) and decrease or disappearance of certain leucocytes from bone marrow (agranulocytosis).
Severe Disease
Antibiotics
The use of antibiotics may sometimes be necessary, but its continued use will kill off the intestinal microflora required for good health, and will open the way for organisms-of-opportunity, such as the yeast/fungus Candida albicans.
The effects of an overgrowth of intestinal fungal candidiasis will create additional physical problems, as well as mimic many other physical ailments.
One problem further that Candidiasis creates is an increasing number of food allergies which not only create their own brand of ailments, but can also mimic other physical problems, including this one.
Corticosteroids
Large doses of corticosteroids results in a deficiency of lymphocytes in the blood, leading to lymphopenia. Large leucocytes, called "monocytes," show an impaired ability to kill invading microorganisms.
Corticosteroids interfere with a variety of functions, not mentioned here, and the result of all of the adverse phenomena is an increased incidence of infection usually controlled by cellular immunity, which means an increase in infections of mycoplasm, yeast/fungal, bacterial, protozoal, and so on.
The list of microorganisms resulting from the use of corticosteroids resembles the agents to which patients with Hodgkin's disease or acquired immune deficiency syndrome (AIDS) are vulnerable.
Steroids are also widely used in organ transplants involving kidney, heart, liver and bone marrow. In part, subsequent infections that are news-media-wise blamed on infections after transplantations are a direct result of use of the corticosteroids as well as other immunosuppressive drugs.
Other Necessary Treatments
Combating emergency kidney problems – as with the use of kidney dialysis – and other system problems, may, however, be very necessary expedients, but should not be considered as lifelong limitations.
Alternative Treatments for Systemic Lupus Erythematosus and Progressive Systemic Sclerosis
Anti-Amoebic (Anti-Microbial) Treatments
Gus J. Prosch, Jr., M.D.15 uses The Arthritis Trust of America/The Rheumatoid Disease Foundation recommended treatment with beneficial results.
Anti-Fungal, Anti-Mycoplasmic Treatments
According to Dr. Costantini,15 by treating various so-called auto-immune diseases with anti-fungals, including Systemic Lupus Erythematosus, the disease can be halted.
Among the traditional antifungal drugs are found lovastatin, griseofulvin, ketoconazole, neomycin, fibrates, tetracycline and others, some of which may also be effective against Lupus. However, these should all be administered by a health professional, with due consideration for their adverse effects, including that of killing off beneficial microbes – Lactobacillus acidophilus – in the intestinal tract.14
Boron - The Case of Johnny Reebuk
Dr. Rex E. Newnham, N.D., D.O., Ph.D.13 describes an old soldier who was being treated for Systemic Lupus Erythematosus in Brisbane Veteran's Hospital, Australia, but was not being helped by traditional treatments.
Johnny's main symptoms were pains in the muscles and joints with some red blotches on the skin. He came to Dr. Newnham for help, and was given Osteo-Trace® tablets containing 3 mg of boron, and also a zinc supplement for his skin. Within 2 months Johnny was very much better, and he continued the treatment for another 3 months. Two years later, he was still well.
Chiropractic
A case of Systemic Lupus Erythematosis is reported by Paul A. Goldberg, M.P.H., D.C.,18 graduate of Bowling Green State University, Life College and the University of Texas Medical Center Graduate School of Public Health. Dr. Goldberg holds degrees in preventive medicine, nutrition and chiropractic, and is Professor of Clinical Nutrition, Gastroenterology, and Rheumatology at Life College in Marietta, Georgia. He operates The Goldberg Clinic in Marietta, Georgia.
The Case of Cathy Huxoll – Cathy Huxoll, 29-years-of-age, had a 10 year history of severe fatigue, joint pains, skin problems, and immune dysregulation. She'd been diagnosed with Systemic Lupus Erythematosus, and undergone years of corticosteroid and methotrexate usage. Cathy said her condition was "desperate" and she was on the verge of suicide.
Cathy's husband, a medical physician, tried to dissuade Cathy from consulting with a Chiropractor as they had "nothing of any usefullness for her condition outside of the drugs that she was already taking."
When Cathy appeared in Dr. Goldberg's office she appeared weak, pale and had very poor muscle tone. She'd also had been convinced over the years that her condition was permanent and would only get worse in time, something of a self-fulfilling prophecy.
Dr. Goldberg worked to convince her that she could be optimistic, although recovery might be slow and difficult.
Cathy was anemic, low in amino acid levels, had abnormal bowel flora and was on a diet of refined carbohydrates, coffee, and fast foods. She had numerous food and inhalant allergies. Blood sugar levels were erratic and there were multiple vitamin and mineral deficiencies along with general body toxicity.
Cathy was placed on a dietary reform with elimination of allergens and refined carbohydrates. Specific supplements were given to assist in removing toxic minerals. She was advised to avoid future dental silver/mercury amalgams and to consider replacement of those she had with composite fillings. An amino acid blend was constructed based on her laboratory findings. She was advised to eat whole foods, and provided with other supplements to improve functioning of her body as a whole and the immune system specifically. Acupressure was employed, and the patient began training in meditation and relaxation disciplines.
Cathy's first several weeks were rough. She missed the stimulation of her coffee and junk foods and suffered withdrawal symptoms as she avoided her food allergens. Within two months she began to notice improved energy and a decrease in muscle and joint pain. Her skin began to improve and her color became more healthy. Encouraged by the improvements, the patient doubled her efforts and continued to reap health rewards. Cathy gradually ceased taking steroids and methotrexate.
Four years later Cathy is pursuing a nursing career and enjoys good health and freedom and has only occasional mild joint discomforts which she describes as "very minor in nature."
Diet
As with virtually all health conditions the "cave man" diet is recommended, at least modified as best possible. Additional suggestions from Alternative Medicine: The Definitive Guide,3 include (1) avoid overeating, (2) limit cow's milk and beef products, (3) increase green, yellow and orange vegetables, consume non-farmed cold water fish several times a week, (4) avoid alfalfa sprouts or tablets which contain Lcanavanine sulfate which can aggravate Lupus, (5) avoid L-tryptophan supplementation, that might promote autoimmune processes.3
One should also assess and treat for candidiasis, food allergies and chemical sensitivities.3
Enzyme Therapy
Enzyme supplementation, along with proper diet, may be very important for properly digesting food, and for eliminating the inflammatory immuno-complexes that always accompanies Systemic Lupus Erythematosus.
Dr. Catherine Russell,21 Guadalajara, Mexico, describes a problem in Mexico which has also long been a serious problem in the United States. Because the Mexican economy has been poor, and although Dr. Russell does not charge much, it's much easier for Lupus patients to get free shots of damaging cortisone, with immediate pain relief, than it is to persist through constructive change of diet, supplements and other remedies. In the United States, it's easier for patients to get "free" or "cheap" treatments through a Health Maintenance Organization or health insurance, where ineffective treatments are dictated by costs, traditional medical practices and insurance dictums, rather than what is necessary for individualized wellness.
Those with Systemic Lupus Erythematosus who stay with Dr. Russell will be given megadoses of vitamin C to assist in getting them off of cortisone (which takes about one month), proteolytic enzymes, B complex, the whole nutritional supplement range and, depending upon where the pain is, she will use intraneural injections and homeopathic remedies.
Fasting
Joel Fuhrman, M.D.,23 reports that "Having fasted over a thousand patients with various diseases I can say without hesitation that fasting is very often the only avenue that a patient can use to establish a complete remission.
"This is especially true with autoimmune illnesses like lupus where it is almost impossible to shut off the hyperactive immune system with nutritional modifications alone, without total fasting.
"[The] failure to understand the benefits of fasting, stems from a narrow perspective, viewing fasting as merely a means to enhance detoxification, ignoring the other pathophysiologic mechanisms involved in most chronic degenerative diseases. The body clearly has the mechanism to adequately handle the removal of endogenous wastes generated in the fasting state. In fact, fasting has been shown to improve or normalize abnormal liver function."
It is adviseable to refrain from the use of drugs and other chemical exposures during fasting.
Herbs
According to Burton Goldberg's Alternative Medicine: The Definitive Guide,3 "Mix equal parts of the tinctures of the Chinese herbs Bupleurum falcatum, licorice, and wild yam. Take one teaspoonful of this mixture three times a day. Drink an infusion of nettle twice a day. In addition, as this autoimmune condition can manifest with a range of symptoms, this should be treated with the relevant herbs as they arise: Echinacea, goldenseal, pau d'arco, red clover."3
Hormonal Replacement Therapy
A proper functioning hormonal system is a requisite for good health, and often a deficiency in thyroid will accompany Systemic Lupus Erythematosus.
Mineral Infrared Therapy
Dr. Tsu-Tsair Chi has reported on an infrared cermic-coated device that has beneficial effects in strengthening the immune system, decreasing pain, unblocking lymph channels, increasing circulation, and providing lacking trace elements. The Mineral Infrared Therapy device is worth trying for Systemic Lupus Erythematosus.12
Nutrition and Supplements
According to Johnathan Wright, M.D., world reknown nutritionist from Kent, Washington, (1) Vitamin B6 as high as 500 mg three times daily can be very useful in reducing symptoms; (2) more than 80% of Lupus sufferers are lacking in hydrochloric acid, and need supplementation; (3) all Lupus patients have food allergies, and will improve when this condition is handled; (4) more than 50% of women have dehydroepiandrosterone (DHEA) and testosterone levels lower than other women, and they need these deficiencies replaced via hormonal therapy.3 (See Jonathan V. Wright, M.D., "Treatment of Lupus," and Alan R. Gaby, M.D., Nutrition and Healing.)
Other supplements may include vitamin C and bioflavonoids, proteolytic enzymes (away from meals on empty stomach), digestive enzymes with meals if necessary, calcium/magnesium, zinc, essential fatty acids, amino acids such as L-cysteine, L-methoionine, L-cystine, beta-carotene and vitamin A, vitamin E (1,500 I.U. daily), garlic capsules, vitamin B complex, vitamin B5, vitamin B12 intramuscular injection (1,000 mcg intramuscular two times weekly), and selenium.3
The Case of Angela Boynton – When Angela Boyton, 34-years-of-age, sought out the assistance of Jonathan V. Wright, M.D.17 for her lupus, she was determined to avoid damaging, traditional treatments, and to do whatever necessary to get well. She'd already read up on books about nutrition and had a pretty good idea about the so-called "cave-man" diet, having restocked her kitchen with whole foods, whole grains and eliminated flour, artificial flavors, colors, preservatives, sugar, artificial sweeteners, hydrogenated or partially hydrogenated oils, and she used practically no canned stuff. She also had worked up her vitamin C intake to "bowel tolerance level."
Angela was on the right track, but Dr. Wright restricted her diet even further, adding in precautionary laboratory tests and additional supplements.
A 24-hour urine test was made for excess oxalate because occasionally the excess is associated with taking large amounts of vitamin C, and can contribute to stone formation which might damage the kidneys. "As you know," Dr. Wright cautioned, "kidneys are a potential weak point in lupus.... Since 1973, I've only seen oxalate kidney stones associated with high-quantity vitamin C twice."
Dr. Wright agreed that permanently eliminating non-foods – foods that have been processed, packaged or otherwise treated after leaving the garden – was an "absolutely necessary step for optimal health."
Dr. Wright also eliminated 100% of Angela's wheat, oats, barley, rye and any other grains that might contain gluten and gliadin, proteins found in all grains except corn and rice.
Food sensitization tests were made and, where possible, a desensitization program was begun. Dr. Wright explained that "people who have lupus, ulcerative colitis, Grave's disease, juvenile diabetes, vitiligo, and several other 'autoimmune' diseases very frequently share tissue types (genetic markers: HLA types B8, DR3, and DR4) that are also common to celiac disease, the disease caused by gluten and gliadin.... The folks with lupus I've worked with have found it very important, along with permanent elimination of cow milk and diary products."
As stomach acid and pepsin are usually low in people with lupus, tests are made for these two, and where required, hydrochloric acid and pepsin capsules are supplemented.
Also Dr. Wright would inject many of the nutrients such as B-vitamins and minerals.
B6 is given, 500 mgs three times a day, because almost "all the drugs that can cause lupus and lupus-like symptoms severely inhibit enzymes that depend on B6," which also, as a side bonus, inhibits the formation of oxalates.
At least one teaspoon of flax-seed oil, along with gammalinolenic acid (GLA) should be taken daily. "Primrose, black currant and borage oils are all good. Make sure there's a total of 240 mgs GLA daily." (As the name "primrose," is not a controlled name, and some unscrupulous packagers use soy-bean oil instead of the proper oil, be sure that you purchase from a reliable dealer, or purchase the brand recommended by your health care provider.)
Angela was advised to take 800 units of vitamin E to help the metabolization of essential fatty acids and also to take 30 mgs daily of zinc (picolinate).
As Angela felt that she was sensitive to the vitamin E she'd already taken, Dr. Wright said that he would either desensitize her, or help her find a form with which she was not sensitive.
Angela could not quite understand why she would need hormone treatment at her age (34), but Dr. Wright explained that it wasn't female hormones that the lupus patient might lack, but rather the important precursor, DHEA (dehydroepiandrosterone) and the male hormone, testosterone, as these two are usually of lower-than-normal levels in lupus sufferers. More tests, of course, were to be made to ascertain facts.
Dr. Wright reports that "It's been nearly seven years since Mrs. Boynton's first visit. Although it took her over a year and a half to get all these factors under control and working for her, she's been symptom free for the last five years."
Richard A. Kunin, M.D. Treatments
Richard A. Kunin, M.D. controls inflammatory responses by use of Omega-3 essential fatty acids, such as those found in cod liver oil and a good grade of flax oil. "Anti-histamines, including certain bioflavonoids, offer additional anti-inflammatory benefits. Vitamin E, selenium and vitamin C also can be very helfpful if used promptly, so as to minimize joint deformity. Doses as low as 40 mg per day can take the heat out of the tissues if the support nutrients are given. Vitamin A is the most important of the vitamins, since it is so often depleted in people with relapsing auto-immune disease – healing and repair require vitamin A, which is depleted in many people who have been ill or have had infections."10
Oxygen Therapies
A modern pioneer in a method of treatment centuries old, Charles Farr, M.D., Ph.D.,9 of Oklahoma City, Oklahoma, was able to prove that the good effects from the use of hydrogen peroxide intravenous infusions were due to its ability to stimulate oxidative enzymes, returning them to normal.
Other scientists and researchers had long ago proven that hydrogen peroxide used both internally and externally can kill foreign microbial agents and, in fact, our macrophages – an important part of our defensive system against infection – routinely manufacture and use hydrogen peroxide to kill microbial agents.
Dr. Farr, and other physicians, use hydrogen peroxide for a wide range of health conditions, among which are AIDS, arthritis, cancer, candidiasis, chronic fatigure syndrome, depression, Systemic Lupus Erythematosus, emphysema, multiple sclerosis, varicose veins and fractures.
According to Dr. Farr, many other conditions besides these will also be benefited.3
There is also ozone therapy and photophoresis applicable to treating many conditions.
Qigong for Arthritis
The balancing of the distribution of biolectrical energy to body parts in need can be an important therapy.16
Roger Jahnke, O.M.D., Santa Barbara. California, has successfully treated a number of Systemic Lupus Erythematosus patients. Using Chinese medicine, including acupuncture, herbal supplements, and Qigong, his patients have been able to solve this degenerative problem.35 (See Roger Jahnke, O.M.D., books, Qigong: Awakening and Mastering the Medicine Within, The Self Applied Health Enhancement Methods; tape, Deeper Relaxation for Self Healing and Dr. Yang Jwing-Ming, Qigong for Arthritis.)
The Remarkable Ronald B. Davis, M.D. Treatment
The Case of Maria Aladante – Maria Aladante, 37 years-of-age, was diagnosed as having Systemic Lupus Erythematosus at a Houston, Texas medical center. Pain in her hands and fingers kept her from performance of her duties as a court reporter.
When she came to Ronald M. Davis, M.D.20 she was given the same treatment as described for Suzie White at the beginning of this article.
Within twenty intravenous infusions Maria began regaining the use of her hands and fingers. Sjogren's syndrome – a marked dryness of all mucous membranes resulting from deficiency of glandular secretions in the throat, salivary glands, upper respiratory tract, sweat and stomach glands – also began to resolve.
With continued intravenous infusions and physical therapy, Maria returned to her court reporter functions, with no restrictions, and she has remained medication and symptom free.
The Case of Alice Wilson – Alice Wilson, 65 years-of-age, was diagnosed with Systemic Lupus Erythematosus at a medical school near Ronald M. Davis'20 office, and placed on traditional treatments of cortisone, cytotoxic drugs and so on.
Dr. Davis used essentially the same treatment as already described for Suzie White, with alternation between EDTA/DMSO and hydrogen peroxide intravenous infusions.
Response was immediate and Alice has done well, currently off all medications expect aspirin and tylenol for mild pain. Alice has returned to all normal activites and no longer suffers from Lupus symptoms.
Universal Oral Vaccination
Early research with Rheumatoid Arthritis and "Rheumatism," involved staphylococcus and streptococcus killed organisms injected as antigens, the successful results thus strongly supporting the infectious nature of Rheumatoid Arthritis. As many forms of Rheumatoid Disease seem to have an infectious and/or allergenic component, such as Ankylosing Spondilitis, Candidiasis, Crohn's disease, Fibrositis, Fibromyalgia, food allergies, rhinitis, and so on, this form of protection may be not just all-inclusive, but also cheap and all-important.
Drs. H. Hugh Fudenberg and Giancario Pizza,22 using a substance related to the "immune milk" derived from a cow (as reported elsewhere) – dialzyable leucocyte extract/transfer factor - "13 of 34 patients improved considerably, despite the fact that they received only two injections the first week and one injection weekly for one month, then one injection monthly for the following five months."
Part 2: Progressive Systemic Sclerosis (Scleroderma)
The Case of Mrs. Rodriguez
This fifty-five year old Mexican lady had tightness and swelling of her face, hands, arms and feet. Her symptoms had begun approximately one year prior to coming to Ronald Davis, M.D.18 of Seabrook, Texas, for treatment.
She'd had surgery on her right wrist for Carpal Tunnel Syndrome, and was supposed to have the other wrist operated on, too, but since she had not improved from the first surgery, it was decided not to operate on her other wrist.
Mrs. Rodriguez had difficulty moving hands and fingers, the fingers being fixed in a mild degree of flexion. She was unable to close her fists.
The skin of her hands and arms was darkened and very firm and painful to touch. Her feet and toes were similar to the hands, as the toes could not be moved, and were swollen. The skin of her feet and legs, to her knees, was darkened similar to that of her arms.
The skin on her arms and legs had a glistening, shiny, slick appearance.
She was successfully treated by The Arthritis Trust of America/The Rheumatoid Disease Foundation so-called "anti-amoebic" therapy, as well as dimethylsulfoxide intravenous (DMSO) infusions4,5 with intravenous ethylene diamine tetracetic acid (EDTA) therapy and hydrogen peroxide intravenous infusions.3,4,5,6
What is Progressive Systemic Sclerosis?
Systemic Sclerosis (Scleroderma) is a thickening of the skin by formation of fibrous tissue, and by changes in internal organs that accompany the thickening tissue changes.
Causation of Progressive Systemic Sclerosis
The cause of this disease is considered to be unknown, but it is considered probable that some form of skin (endothelial) injury starts the sequence of events that results in multiorgan involvement.
According to A.V. Costantini, M.D.,12 a list of diseases wherein fungal forms of microorganisms have been found include the following: atherosclerosis, cancer, AIDS, diabetes mellitus, Rheumatoid Arthritis, Sjogren's syndrome, Systemic Lupus Erythematosus, Gout, Crohn's disease, multiple sclerosis, hyperactivity syndrome, infertility, psoriasis, cirrhosis, Alzheimer's disease, Scleroderma (Progressive Systemic Sclerosis), Raynaud's disease, sarcoidosis, kidney stones, amyloidosis, vasculitis, and Cushing's Disease.
Distribution of Progressive Systemic Sclerosis
Scleroderma is four times more commen in women than in men, and is found in all racial groups and all geographic regions.
Perhaps 12 persons per million per year are diagnosed with this disease, but many investigators feel that the frequency is greater, as it is often mis-diagnosed as Raynaud's disease, a condition that involves capillary congestion and swelling especially of the extremities.
Disease onset is greatest between ages of 25 and 50, although all age groups can be affected.
Clinical Symptoms
Initial symptoms: capillary congestion and swelling, especially of the extremities (Raynaud's phenomenon); gradual thickening of the skin of fingers; joint inflammation, several (polyarthralgia); muscle weakness, indistinguishable from polymyositis (sclerodermatomyositis); segmented cellular death and inflammation of small and medium arteries and deficiency of blood in tissues supplied by these arteries (polyarteritis); visceral disturbances;
Progression of Disease: dilation of capillaries form tumor cells which Tend to form blood and lymph vessels on fingers, face, lips and tongue; face becomes masklike; other vascular, liver and lung problems may occur; skin becomes taut, shiny and pigmented; subcutaneous calcifications develop, usually on fingertips and over bony eminences; symmetric hardening of skin, possibly confined to fingers or other remote body parts.
The best survival outcome is for children, where statistics indicate a survival rate of 90% over ten years or more, although they often develop inflammation of arteries (arteritis) involving the gastrointestinal tract.
Initial Diagnosis
The most common symptom, in 70% of patients, is "Raynaud's phenomenon" which involves capillary congestion and swelling of the extremeties, along with a gradual thickening of the skin of the fingers.
More than one joint may become painful, known as "polyarthralgia."
In some cases there is a muscle weakness, as the predominant feature, and this characteristic is indistinguishable from a condition called "polymyositis," although when found in Scleroderma it is given the name of "sclerodermatomyositis."
Thickening and hardening of the skin, due to collagen tissue accumulation in the lower part of the skin (dermis), tends to be symmetric and may be confined to fingers or distant parts of the upper extremeties; or, the hardening can affect almost all of the body.
Progression of the Disease
As the disease progresses, the skin may become taut, shiny, and over pigmented.
The face becomes masklike.
Small tumors (angiomas) may appear on the fingers, face, lips and tongue.
Calcifications may develop below the skin more commonly in women, usually on the fingertips and over bony eminences.
Biopsies will show increased collagen fibers beneath the skin, along with thinning of the outer skin (epidermal) layers, and certain kinds of atrophy. Swelling of the fingers, while painless, may be accompanied by symptoms of morning stiffness, joint pains (arthralgia), and Carpal Tunnel Syndrome.
Internal organs will also lose their proper functioning, usually paralleling observable skin changes. Changes may restrict themselves to a cluster called the CREST Syndrome, named after the characteristic symptoms of calcinosis, Raynaud's phenomenon, esophageal dysfunction, sclerodactyly (fingers and toes), and telangiectasia (dilation of capillaries and minute arteries, forming a variety of tumors), all names given to various ones of the above described symptoms.
Other visceral changes develop, which characteristically include organ changes caused by vascular deficiencies of the lung and liver.
Joints and tendons become painful due to friction rubs, particularly of the knees and through the tendon sheaths.
Flexion contractures occur at the fingers, wrists, and elbows resulting from fibrosis of the synovium and the tissues surrounding joint structures.
Ulcers may become common, especially at the fingertips and overlying finger joints.
Esophageal dysfunction is the most frequent visceral change, including difficulty in swallowing (dysphagia) and acid return flow (reflux)
Decreased mobility of the small intestine may also be associated with malabsorption resulting from anaerobic bacterial overgrowth. (Anaerobic bacteria are those that can live in an oxygen-free environment.) There may also be degeneration of the mucosa, and entry of air into the submucosa of the intestinal wall.
Large-mouthed sacs develop in the colon and ileum where muscle tissue atrophies.
Fibrosis of the lungs causes defective gas diffusion. Inflammation of the lining surrounding the lungs and heart may also occur.
Heart arrhythmias and nerve conduction disturbances and other cardiac abnormalities may occur. Cardiac problems tend to develop and can reach heart failure.
Severe kidney disease may develop.
Rheumatoid Factor (RF) tests are positive in a third of patients. Antibody tests (serum antinuclear or antinucleolar antibodies) are positive in 60%.
Patients with Scleroderma will often have mixed connective tissue disease, and will show clinical and blood tests of Scleroderma as well as muscle inflammation (myositis), anemia, abnormal lowering of white blood cell count (leukopenia) and other positive signs of Systemic Lupus Erythematosus.
Clinical changes are sometimes very slow, the progress of the disease becoming unrecognizable from year to year.
A medically defined "generalized" condition of the disease involves assessment of the presence of skin thickening on the chest and abdomen.
A medically defined "limited" condition involves skin changes to sites such as the wrist, ankles and clavicles.
After a long period (ten years) an improving medically defined "generalized" disease or a medically defined worsening "limited" disease becomes undistinguishable.
Early deaths usually involve, bacterial infections, pneumonia, malignancy, or heart involvement.
Associated Conditions
Associated medical conditions depend upon organs affected, and the symptoms produced by the specific organ dysfunction. Certain organs – endocrine glands, gastrointestinal tract, kidneys, and lungs –occur frequently, with corresponding difficulties.
Generally there may also be joint pains (arthralgias), Carpal Tunnel Syndrome, congestive heart failure, thyroid deficiencies (Hashimoto's thyroiditis), inflammation and degneration of connective tissue (Polymyositis), malignant tumors (neoplasms), deficiency in secretion of tears (Sjogren's syndrome), Raynaud's phenomena, Rheumatoid Arthritis, and Systemic Lupus Erythematosus.
Traditional Treatments
No traditional treatments have been shown to be effective.
Corticosteroids are used to alleviate symptoms.
As with Rheumatoid Arthritis, various forms of D-penicillamine and cytotoxic immunosuppressive drugs – such as methotrexate – are used.
Feeding problems are usually addressed by advising the patient to take small feedings, more frequently.
Tetracycline and other broad-spectrum antibiotics are used to suppress the intestinal microflora, to hopefully alleviate symptoms of intestinal malabsorption.
Physiotherapy is used to preserve muscle strength, but is ineffective in preventing joint contractures.
What's Wrong With Traditional Treatments
No traditional treatment attempts to step outside of known, already failed modalities.
Corticosteroids
The most dramatic, short-lived relief may come from corticosteroids, drugs that dramatically relieve pain, swelling, and heated joints for a short period. When first discovered, it was hailed as the panacea for the arthritic, and then it's many damaging effects became known.
Steroids, or their analogs (triamcinolone hexacetonide; prednisolone tertiary-butylacetate) were, and are, given orally, as prednisone, by injection into the joints themselves (intra-articular), or at specific sites, especially near connections of tendons, ligments, and other locations near joints.
Although corticosteroids dampen down the clinical symptoms and permits temporary freedom of movement without pain, their usage is, or should be, restricted because of many damaging side effects.
D-Penicillamine
D-penicillamine is, at best, a routinely used "experimental drug," and has never been shown to heal anyone, or bring about any kind of remission.
Immunosuppressive Drugs
Usage of cytotoxic drugs such as methotrexate is an attempt to change the course of an immune system presumed to have gone awry.
These are drugs that are routinely used in the treatment of Tetracycline
The continued usage of antibiotics, including tetracycline, for the purpose of controlling unwanted organisms-of-opportunity in the gastrointestinal tract, is doomed to long-term failure for at least two reasons: (a) the usage of antibiotics itself, destroys the "good guys" microflora, Lactobacillus, acidophilus, so necessary to human digestion and nutrition, thus allowing organisms-of-opportunity to take root in the mucosa of the intestinal tract, thus appearing to require more administrations of antibiotics; (2) there is no attempt during administration of antibiotics to replace the "good guys" Lactobacillus, acidophilus microflora.
In the presence of renal or liver dysfunction, particularly in pregnancy, 2 grams or more taken daily intravenously has been associated with deaths. Even oral dosages can be damaging.
There are many additional adverse effects possible when using tetracycline, including gastrointestinal, skin, hypersensitivity reactions, and blood.9
Small Feedings, Taken Frequently
While small feedings, frequently taken, may be a necessary evil, there is apparently no attempt to correct the situation that makes this evil necessary, nor to guide the patient through a truly constructive dietary regimen.
Non-Traditional Treatments
Anti-Amoebic (Anti-Microbial) Treatments
Gus J. Prosch, Jr., M.D., Alabama, reports that he effectively treats his Scleroderma patients exactly the same way as he does his Rheumatoid Arthritis patients.
Anti-Fungal, Anti-Mycoplasmic Treatment
According to Dr. Costantini,15 the concept of auto-immune diseases contains a fatal flaw, because no successful species can develop a system of defense which attacks itself. "No species of life can make an antibody against itself; particularly causing fatal disease such as Scleroderma."
Antibodies that are measured in the blood stream and which imply an autoimmune condition are actually antibodies against "ubiquitin," a substance that is present in many species including that of fungi.
"Scleroderma responds well to the antifungal agent griseofulvin."
It has also been reported that colchicine is a good anti-mycotoxin, which may be one of the reasons why Gouty Arthritis responds to administration of colchicine
Other possible antifungal antibiotic agents have similar action to colchicine. Reported by Dr. Costantini are also lovastatin, griseofulvin, ketoconazole, neomycin, fibrates, tetracycline and others, some of which may also be effective against Scleroderma. Care must be taken that these are administered under the supervision of a health professional, and that Lactobacillus acidopholus replaces the intestinal microorganisms bound to be destroyed.
Boron
The Case of Sister Theresa – Sister Theresa, suffering from Progressive Systemic Sclerosis, lived in a retirement convent in Pietermaritzburg, South Africa. She was very stiff and unable to handle stairs properly. In order to go downstairs she had to sit on each step and bounce down to the next on her buttocks. "It was truly a traumatic process," Dr. Newnham11 reports, "to see her go downstairs."
Sister Teresa was given boron tablets with 3 mg of boron in the form of Osteo-Trace®, and in three months she could walk up and down stairs properly.
She is now 84-years-of-age.
Detoxification and Nutritional Support
According to Mark Davidson, D.O., N.D.15 (also trained in Chinese medicine and acupuncture), an ideal clinic would address the whole person, not just components that make up the person. Dr. Davidson says that "So many people say they've got the cure, they've got the whole picture. I tend to see little parts of a puzzle. You get a better picture when you get more viewpoints.... We look at the patient's physical, emotional, electromagnetic, biochemical and spirtual being, using a team of experienced practitioners, each contributing their health expertise in a particular area but applying it in such a manner that the whole individual is treated."
The Health Regeneration Clinic near Waynesville, North Carolina, handles all forms of degenerative diseases, including arthritis and cancers. The following is a brief description of their treatments:
The patient is placed in an environment conducive to peace and serenity surrounded by woods and forests with pure water, fresh air, bio-dynamic gardens, and a spring-fed, solar-heated swimming pool.
Dr. Davidson, and the other health-care professionals, believe that how a person thinks influences their emotions and physical conditions. "In treating degenerative problems, our emphasis is on our modern way of life. Change of habits and patterns that get to the core of things. If you can advise people on how to handle stress factors in their life, relationship factors, communication skills, work problems, you're looking at a multi-factorial approach in dealing with stress." If a person's beliefs, thoughts and emotions are chaotic, scattered, or confused, they will have a difficult time healing. "The physical problem is the end-stage of unresolved, strong emotions." Staff members help clients confront the issues that they need to address.
As most people with chronic illness have major toxicity problems, usually stemming from the bowels, Dr. Davidson believes that cleansing of the bowels is of primary importance. This is done by means of fiber, herbs, enzymes and nutrients, plus colonic irrigation. Dr. Davidson says that "Usually toxicities found in the gallbladder, liver and kidneys are cleared only through proper bowel cleansing."
Ozonated colonics and other forms of cleansing will also rid the burden of parasites, of which there are many forms. "This is an important factor, as is getting rid of the lining of the small bowel, because behind the lining you'll usually find a lot of parasites: worms, amoeba, flukes and so forth."
"We also flush out the liver and gallbladder with the use of herbs, nutrients, acupressure, acupuncture, shiatsu (Japanese "finger pressure"), Swedish massage, and by stimulating the lymph system. People who finally deal with their unresolved anger may have a spontaneous detoxification of their liver and gallbladder." (See Burton Goldberg Group, Alternative Medicine: The Definitive Guide, Future Medicine Publishing Co.)
Body tissues are cleansed by using steam cabinets, Turkish baths, herbs that cause sweating, ozonated baths, all of which help toxins to come through the skin. Homeopathic remedies and herbs help to speed up the metabolism and therefore also help detoxification.
After the bowel and organs are detoxified, Dr. Davidson starts giving the right nutrients, preventing additional toxicity from entering into tissues, liver and gallbladder from poor food choices."We also educate people. We teach them about water purity, air pollutants and how to find foods low in or free of toxins, so that when they return home, they can continue their process of detoxification."
As many people develop clogged lymph systems, preventing toxins from being removed from the body, we use lymphatic massage therapy accompanied by a device that combines magnetic therapy with soft laser principles. This is a gentle massage, and it breaks up congealed lymph, permitting the free flow of lymph drainage again. Dry skin brushing is taught, or bouncing regularly on a trampoline-rebounder, as these will also help lymph to drain.
"Most chronically ill people have toxin-producing infections," Dr. Davidson believes. "This stems from root canal teeth or previous tooth extractions. As these infections are tied in with acupuncture meridians which pass through internal organs, these organs are also affected. Therefore it's important to clean out pockets of dental infection and 'dead' teeth."
Uneven bites or malocclusions – where teeth do not match up perfectly – can also affect health. Muscles on one side of the jaw create stress to the cranium, neck and back, producing mis-alignment in the cranial-sacral region, and this can affect many other internal organs.
As mercury amalgam is one of the primary sources of accumulated toxicity and immune suppression, these fillings should be considered for replacement. Such fillings also create unhealthy electromagnetic effects resulting from the chemical/electrical activity of two dissimilar metals (mercury and silver). Like a small battery, a constant current is created from the acid/alkaline pH of the saliva. Current, which creates a flow of electrons, also creates a magnetic field which influences release of certain hormones and neurotransmitters, affecting bodily functions. The electro-chemical action can also disassociate otherwise harmless chemicals, creating a cumulative toxic condition.
A dentist is provided to assess and to solve these otherwise hidden problems.
Although not necessarily related to teeth, geo-magnetic fields (geo-pathic lines) can also influence a persons health, and education is important to avoid certain electromagnetic stress.
Once there is sufficient metal removed from the teeth, intravenous chelation therapy is used, starting with di-mercaptopropane sulfonate (DMPS), which attaches to and removes bi- and tri-valent metals such as mercury, lead, arsenic, copper, cobalt, chromium, cadmium, and silver. After this, ethylene diamine tetracetic acid (EDTA) is used as a chelator. This substance attaches to the calcium that holds atherosclertic plaques together, allowing them to dissolve and flush from the body, thus opening up as much as 80% of the peripheral circulation, providing improved cellular nourishment and oxygenation.
Dr. Davidson says that "These approaches must be combined with changes in the person's diet, lifestyle, and nutrient supplementation. One of our prime goals is for people to come to our clinic, learn the techniques, and take them back home to use and to show others. We're not interested in treating diseases, but in building health."
Enzyme Therapy
Enzyme supplementation, along with proper diet, may be very important for properly digesting food, and for eliminating the inflammatory immuno complexes that always accompanies Progressive Systemic Sclerosis.
Herbs
As reported in The American Journal of Natural Medicine, in a study of 13 female patients with Scleroderma, oral administration of 20 mg of Centella asiatica (Gotu Kola) given 3 times daily, was very successful in 3, successful in 8, and unsuccessful in only 2 out of 13. "Improvement consisted of decreased skin hardening, reduced joint pain, and improved finger mobility."14
Mineral Infrared Therapy
Dr. Tsu-Tsair Chi has reported on an infrared cermic-coated device that has beneficial effects in strengthening the immune system, decreasing pain, unblocking lymph channels, increasing circulation, and providing lacking trace elements.10
Qigong for Arthritis
The balancing or distribution of biolectrical energy to body parts in need can be an important therapy.13
The Case of Carlene Charles – Roger Jahnke, O.M.D.,17 Santa Barbara, California, has had several cases of Scleroderma. Carlene Charles, in her early 30s, was one of his most brilliant patients, as she stated up front that she was going to have a team of health care providers, and that she was not going to buy in on the idea that Scleroderma was going to kill her.
"Her physician, who is a reasonable primary care provider, encouraged her to follow her desire to use Chinese medicine, herbs, acupuncture, etc.
"After about four years Carlene arrested her disorder. There was a point where her mouth and her face began to show Scleroderma signs, and she actually recovered from that – both face and feet actually recovered from moderate stage Scleroderma signs, however her hands only partially recovered.
"Her hands only partially recovered, but she's working on it."
Ronald Davis, M.D. Remarkable Alternative Treatment
More on Mrs. Rodriguez – When Mrs. Rodriguez came to Dr. Davis for help – as reported at the beginning of this chapter – she had all the symptoms of Progressive Systemic Scleroderma, a disease that Dr. Davis had previouslytreated successfully, just as he had treated Rheumatoid Arthritis and Systemic Lupus Erythematosus successfully.
Medications taken by Mrs. Rodriguez under traditional treatments were 2 tablets of acetaminophen with codeine, 4 tablets 6 times per day; 1 tablet of Tylenol, 500 mg each 4 hours, 1 250 mg tablet of Pen V-K each 6 hours; Procardia caps, 10 mg 3 times each day; 250 mg tablet of hydroxyzine 4-6 hours as needed with itching; 250 mg Cuprimine capsule 2 times daily; 400 mg Ibuprofen capsule 3 times daily; 10 mg Flexeril 1 tablet 2 times daily; 300 mg Tagamet 2 tablet 3 times daily; 150 mg Zantac 1 tablet 3 times daily.
Mrs. Rodriguez had difficulty moving her hands and fingers, the fingers fixed so that she could not close her fists.
Skin on the hands and arms were darkened and very firm and painful to touch.
Feet and toes, similar to her hands, could not easily be moved, and were swollen.
As described in the section on Systemic Lupus Erythematosus, Dr. Davis started the patient with (1) The Arthritis Fund/The Rheumatoid Disease Foundation's recommended anti-amoebic treatment, and also began (2) dimethylsulfoxide intravenous (DMSO) infusions4,5 with intravenous amino acid ethylene diamine tetracetic acid (EDTA) therapy.3,4,5,6 (3) Dr. Davis also later administered intravenous infusions of hydrogen peroxide (H2O2).8
Only a moderate Herxheimer7 effect (organism die-off effect) was noted on the first two medications of the anti-amoebics, and was hardly noticeable on the next four treatments.
Intravenous infusions of dimethylsulfoxide intravenous (DMSO)4,5 with intravenous ethylene diamine tetracetic acid (EDTA) therapy3,4,5,6 was begun at the same time as the anti-amoebic therapy.
After the first month, hydrogen peroxide (H2O2)8 was used in place of the dimethylsulfoxide intravenous (DMSO)4,5 with intravenous ethylene diamine tetracetic acid (EDTA) therapy.3,4,5,6
Mrs. Rodriguez's improvement was quite evident during the following year. Her hands, arms, feet and legs began to soften within the first week of treatment.
She felt that the hydrogen peroxide (H2O2) made her "itch on the inside" of her hands, arms, and feet, but the next day after the infusion she felt much better results than she had with the intravenous therapy of dimethylsulfoxide(DMSO) accompanied by intravenous ethylene diamine tetracetic acid (EDTA).
Her condition continued to improve after and between treatments, even when she went 2 to 3 months without treatment.
She had a total of 80 ethylene diamine tetracetic acid (EDTA) with dimethylsulfoxide (DMSO), and 30 hydrogen peroxide (H2O2) infusions.
The skin of her face, arms, hands, legs and feet is now normal in appearance in texture, and she no longer has fatigue and malaise, and her energy and activity levels are normal. She has normal function of her hands and fingers, and is without pain.
The Case of Mrs. Devin – Ronald M. Davis, M.D. of Seabrook, Texas, was approached by fifty year old Mrs. Devin who had been in good health two years prior to to her present health problems, although she'd had the usual childhood illnesses. There were no prior adult illnesses and no surgeries, no history of tuberculosis, diabetes, cardiovascular disease, or hypertension.
She first began to notice a sensation of swelling and tightness of the skin of the face and extremities. These symptoms rapidly progressed to the point of rendering the patient unable to walk, or to do daily household work, as hypertension and headache were early symptoms.
In a year-and-a-half, the condition of the patient deteriorated from mild stiffness of the joints and tightness of the skin, to complete immobilization, with loss of the use of her extremities and loss of flexible facial characteristics. Her fingertips felt coldness and pain.
Mrs. Devin was diagnosed as suffering from Progressive Systemic Sclerosis, a disease that Dr. Davis learned can be successfully treated using the same treatment he had developed for Systemic Lupus Erythematosus.4
She had tightness and hardening of the skin of the body, deformities of the hands, arms, legs and fingers, with an inability to walk, progressive kidney failure, nausea, headache, and fatigue.
One night Mrs. Devin awakened with a sensation of smothering and chest tightness, so she was rushed to the local hospital emergency room, where she was found to have a blood pressure in the range of 200/110. She was given anti-hypertensive medication, and remained on this drug until her final treatments with Dr. Davis.
Kidney involvement was extensive, necessitating dialysis (peritoneal), which she was doing at home with her husband’s assistance. She was also under the care of a rheumatologist and The Texas Kidney Institute at Hermann Hospital in Houston.
Mrs. Devin was unable to perform ordinary household tasks or even to walk as her legs and feet had become stiff and immobile.
Throughout the inevitable progress of her disease under the care of traditional practitioners, she was placed on Compazine, 25 mg tablets 4 times daily for nausea, 2 Dialome, 3 times per day; 1 Capoten 75 mg, 2 times daily; 5 mg prednisone 1 time daily, 0.1 mg Catapres, 1 time at bedtime, and kidney dialysis with 1 liter of solution 4 times daily.
She had been on antihypertensive medications for over one year, and on dialysis for nearly nine months when Dr. Davis first saw her in his office.
During the treatment administered by Ronald Davis, M.D., she responded immediately, and improved continuously. Although it took a year to bring about nearly a complete cure of Mrs. Devin's condition, Dr. Davis' treatment was essentially simple, relying on two parts, as follows: (1) The Arthritis Trust of America/The Rheumatoid Disease Foundation recommended treatment for Rheumatoid Disease; (2) intravenous dimethylsulfoxide (DMSO) infusions6 with intravenous ethylene diamine tetracetic acid (EDTA) therapy.3,7
The first treatment used was 300 mg of allopurinol by mouth three times per day for 7 days, simultaneously with 500 mg of metronidazole, two tablets A.M. and P.M. (2 grams per day) for two consecutive days a week for six weeks.
It’s now been several years since her last treatment. She has full use of her kidneys without dialysis, and was last reported walking about Alcatraz Island on vacation with her husband.
Ronald Davis, M.D., Seabrook, Texas, says, "I truly feel that in order to get complete cure of these rheumatoid diseases, the antiamoebics must be used."
Under this "anti-amoebic" treatment, the patient experienced a severe Herxheimer reaction, including increased nausea, headache and rather severe joint pains, as well as increased muscular aches and pains.9 Moderate relief of these symptoms was obtained by increasing the prednisone by one tablet on the Herxheimer days.
A rather severe Herxheimer continued throughout the six weeks of treatment.
Intravenous treatment using dimethylsulfoxide intravenous (DMSO) infusions4,6 with intravenous ethylene diamine tetracetic acid (EDTA) therapy3,4,7 was begun, and continued periodically for the next two years, gradually tapering off in frequency of administration.
In summary, Dr. Davis uses The Arthritis Fund/The Rheumatoid Disease Foundation's treatment protocol for Rheumatoid Disease (including for Rheumatoid Arthritis), as a starting point, and follows up with intravenous infusions of either (1) ethylene diamine tetracetic acidEDTA/dimethylsulfoxide (DMSO a strong anti-oxidant); and/or (2) hydrogen peroxide infusions.
Dr. Davis reports that he has had "4 cases of Scleroderma which were arrested and all symptoms of Sjogren's syndrome (dryness of mucosal secretions) reversed," using the same protocol as described in this section and the sections on Systemic Lupus Erythematosus and Rheumatoid Arthritis.
"Mrs. Devin is free of symptoms after 8-1/2 years from her last treatment. At last contact, the only medication she is taking is Capoten and Norvasc for residual hypertension. Her kidneys still function well.
"The treatment we use for Rheumatoid Arthritis, Systemic Lupus Erythematosus and Progressive Systemic Sclerosis (Scleroderma) works well in arresting the progress of the diseases as well as reversing most of the skin and organ changes.
"We have had no untoward effects with these treatments except for the pungent odor the patients gets (temporarily) from the DMSO intravenous infusions.
"Sometimes the Herxheimer reaction is severe, but not to the extent that requires discontinuing therapy.
"There have been no untoward effects from the EDTA intravenous infusions, since the dosage is calculated [according to proper standards], given slowly, with close monitoring of blood pressure and blood sugar.
"No patient, to this point, has failed to respond to this therapy."
Cooperative Assistance in This Remarkable Alternative Treatment
Ronald Davis, M.D. received cooperation and assistance in bringing about this remarkable change with the help of Dr. Katy Thompson of the Texas Kidney Institute at Hermann Hospital, Houston, TX, Dr. Stanley Jacobs of the University of Oregon, and also from Charles H. Farr, M.D., Ph.D. of Oklahoma and Garry Gordon, M.D. of Arizona.
Reported by Julian Whitaker, M.D., Stanley Jacob, M.D., world authority on the use of dimethylsulfoxide (DMSO), and one of the national advisors to the Scleroderma International Foundation states that DMSO "is the treatment of choice for both Scleroderma and Raynaud's phenomenon and is beneficial for Rheumatoid Arthritis."16
Universal Oral Vaccination
Early research with Rheumatoid Arthritis and "Rheumatism," involved staphylococcus and streptococcus killed organisms injected as antigens, the successful results thus strongly supporting the infectious nature of Rheumatoid Arthritis. As many forms of Rheumatoid Disease seem to have an infectious and/or allergenic component, such as Ankylosing Spondilitis, Candidiasis, Crohn's disease, Fibrositis, Fibromyalgia, food allergies, rhinitis, and so on, this form of protection may be not just all-inclusive, but also cheap and all-important.
Injecting known, specific allergens or antigens into the cistern (base of teat) of a cow just prior to calving produces protective substances that are curative.
This form of treatment has been shown to be effective with a wide variety of ailments including Rheumatism, Rheumatism, coughing, respiratory problems, sore throat, skin conditions, acne blemishes, upset stomach, cold and flu, diarrhea, and impetigo.
Drs. H. Hugh Fudenberg and Giancario Pizza,20 using a substance related to the "immune milk" derived from a cow (as reported elsewhere) – dialzyable leucocyte extract/transfer factor -"excellent results were obtained ....in 3 cases with Scleroderma, with complete recovery in 2 and considerable improvement in the third."
Part 3: A Treatment for Scleroderma & Lupus Erythematosus
The case that follows applies to Lupus Erythematosus and Scleroderma. It was, for the most part, written by Ronald Davis, M.D.
If you are a victim of one of these terrible scourges, you will most likely wish to present this article to your doctor, or to one of our referral physicians. They will have no trouble reading Dr. Davis’ notes, and will understand fully.
Lupus Erythematosus and Scleroderma are classified as vascular diseases, along with Polyarteritis Nodosa, and some other diseases, but Lupus and Scleroderma also have one other thing in common – they can be treated in a similar manner with equally good results!
Lupus Erythematosus is a chronic, nontuberculous disease of the skin marked by disklike patches with raised reddish edges and depressed centers, and covered with scales or crusts. These fall off, leaving dull-white scars.
Scleroderma is a disease of the skin in which thickened, hard, ridged, and pigmented patches occur. The connective tissue of the skin layer beneath the epidermis (corium) and the subcutaneous structures being increased, a hidebound condition results. The ordinary form begins in middle life, and is often incurable.
The above is according to The American Illustrated Medical Dictionary (W.B. Saunders) given to me by Jack M. Blount, M.D. on his retirement from medical practice.
The Arthritis Trust of America/Rheumatoid Disease Foundation is proud and happy to bring to you a wonderfully successful case history of Scleroderma developed by Ronald M. Davis, M.D., who, we understand, is completing a book on this successful treatment.
The total case history will be reproduced here for those who wish to follow it in detail.
To summarize, this is a report of a case of severe progressive systemic sclerosis in a forty-nine year old white female, who was in good health two years prior to being seen in Dr. Davis’ office. In a year-and-a-half, the condition of the patient deteriorated from mild stiffness of the joints and tightness of the skin, to complete immobilization, with loss of the use of her extremities and loss of facial characteristics. Kidney involvement was extensive, necessitating peritoneal dialysis, which she was doing at home with her husband’s assistance. During the treatment to be described below, she responded immediately, and improved continuously. It’s now been over a year since her last treatment. She has full use of her kidneys without dialysis, and was last seen walking about Alcatraz Island on vacation.
Indeed, her quality-of-life is vastly improved! If she is not cured, then she enjoys an extended remission of all symptoms!
Treatments used were two of our recommended Rheumatoid Disease medications, intravenous EDTA Chelation Therapy, intravenous DMSO Therapy, and Physical Therapy as could be tolerated by the patient.
Since Lupus Erythematosus and Scleroderma, like Psoriasis, have been virtually intractable by traditional treatments, this single success story bears repeating.
But more than this single success story, Ronald Davis, M.D. states and assures us that he has had similar successes with others using the same regimen.
We consider this a breakthrough of the first magnitude, and worthy of your serious consideration, if you or your relatives or friends suffer from either of the above diseases.
The Reversal of Scleroderma (Progressive Systemic Sclerosis)
Initial History and Physical Examination: May 22, 1984
Chief Complaint: Tightness and hardening of the skin of the body, deformities of the hands, arms, legs, and fingers. Inability to walk, progressive kidney failure, nausea, and headache. High blood pressure.
History of Chief Complaint: The patient first began to notice a sensation of swelling and tightness of the skin of the face and extremities about the Spring of 1982. These symptoms rapidly progressed to the point of rendering the patient unable to walk, or to do daily household work. Evidently her kidneys had become affected early in the disease, as hypertension and headache were early symptoms. Patient had been on antihypertensive medication for over one year, and on peritoneal dialysis for nearly nine months, when we saw her in our office. She was under the care of a rheumatologist in Houston and The Texas Kidney Institute at Hermann Hospital in Houston.
Past History: Usual childhood illnesses wihout sequelae (sequela: Any lesion or affection following or caused by an attack of disease), no serious adult illnesses, and no surgeries. No history of TB, diabetes, cardiovascular disease, or hypertension prior to the onset of this disease. Patient is allergic to Demerol.
Family History: Essentially noncontributory, there being no history of the rheumatoid diseases, TB, CA, diabetes, or cardiovascular problems.
Medications:
- Compazine – 25 Mg. tabs 1, four times daily as needed for nausea.
- Dialome – 2, three times per day
- Capoten – 75 Mg. 1, two times daily
- Prednisone – 5 Mg., 1 daily
- Catapres – 0.1 Mg., 1 at bedtime
- Peritoneal dialysis with 1 liter of solution four times daily (prepared by Texas Kidney Institute at Hermann Hospital, Houston.)
Review of Systems:
HEENT: Patient had begun to notice numbness and coldness of tips of fingers, with a sensation of swelling of hands, fingers, toes, arms, and legs about two years ago. The skin of the face, at the same time, became tight and inelastic making facial expressions and movement very difficult, and eventually impossible. No problems with vision or hearing, but had noticed difficulty swallowing recently.
Chest & Lungs: In late 1982 the patient was awakened in the middle of the night, with a sensation of smothering and chest tightness. She was rushed to a local hospital Emergency Room, where she was found to have a blood pressure in the range of 200/110. She was given anti-hypertensive medication, the blood pressure was reduced, and the symptoms abated. She has had to remain on medication for blood pressure control since.
Gastro-intestinal: Negative except for extreme nausea, which has been present since earliest symptoms began in 1982.
Genito-urinary: Patient is Gravida (was pregnant) 5, Para 5 (had 5 children successfully), abortus 0, stillbirth 0. She has five children living, and in good health. She had been on peritoneal dialysis at Texas Institute for past ten months.
Neurological: Negative.
Skin & Extremeties: This condition began with a sensation of coldness and pain of the fingertips. The fingers and hands soon became stiff and immobile, as did the legs and feet. Within six months, the patient was unable to walk or do ordinary daily tasks. She also complained of severe fatigue during the course of this illness, as she had for several months before the first symptoms had begun. The skin and extremities had become slick, shiney, and very hard to the touch within six months after the onset of the first symptoms. The skin of the face was no different.
Physical Examination:
General: The patient is a forty-nine year old caucasian female of Italian extraction in obvious acute and chronic distress from kidney and musculoskeletal disease. (Blood Pressure 140/90, Pulse 94, Temperature 100, Respiration 20, Height 60", Weight 109#.)
HEENT: Head was normal. Eyes: Sclerae and conunctivae were clear, EOM’s (Extra Ocular Movements) intact bilaterally, pupils were equal and equally reactive to light and accommodation. Optic fundi were not examined. Visual acuity was not done. Ears: skin of ears was slick, shiney, and quite tender to touch. Nose: Same. Throat: Throat was clear.
Chest: Lungs were clear to auscultation (listening to lungs) and percussion. The breath sounds were diminished due to shallow breathing from restriction of the rib cage. Heart: Normal sinus rhythm, rate 110 and regular and there were no murmurs.
Abdomen: Thin, symmetrical abdomen, without masses, tenderness, or visceromegaly (enlarged organs) to palpation, and the bowel sounds were normal. Rectal and pelvic exams were not done. The catheters for peritoneal dialysis were in place, there was no sign of infection or irritation.
Neurological: Examination was limited due to immobility of the extremities and tenderness of the skin, but no gross abnormalities of the neurological system were noted.
Skin & Extremities: The skin was white and glistening, and appeared to have been stretched tightly over the bony skeleton. The joints at the elbows, wrists, knees, and ankles were difficult to move. The fingers were fixed in flexion and could not be moved at all. She was the classical Mauskopf face.
Initial Laboratory Data: Hemoglobin 8.4; White Blood Count 7400; Ca++ 9.3; BUN 91; Serum Creatnine 8.3; Glucose 113; Triglycerides 377; Uric Acid 6.6; SGOT 28; SGPT 23; Protein 7.0; Albumin 3.7; Globulins 3.3; LDH 204; Phosphate 4.6; 24 Hr. Creatinine Clearance 7.0; Na+ 140; K+ 5.0; Cl- 100; CO2 24.
Chest X-ray: Negative; EKG: Sinus Tachycardia, otherwise normal Urinalysis: Specific Gravity 1.010; pH 5.0; Protein 1+; Glucose 0; Casts: 2+Red Blood Cell; Bacteria 1+; Red Blood Cell 4-5/high powered field; White Blood Cell 3-4/high powered field.
Impression:
- Severe Progressive Systemic Sclerosis (Scleroderma).
- Nephrosclerosis with kidney failure secondary to scleroderma.
- Severe anemia secondary to 1. and 2.
Treatment Plan:
- The Roger Wyburn-Mason, M.D., Ph.D. Treatment for Rheumatoid Disease
- Intravenous DMSO therapy
- Intravenous Chelation therapy (EDTA)
- Physical Therapy as tolerated by patient
Clinical Course:
On May 22, 1984, the Rheumatoid Disease Foundation therapy was begun in accordance with its protocol, which is as follows: Allopurinol 300 mg. by mouth three times per day for 7 days. Metronidazole 500 mg. – Two tablets A.M. and P.M. two consecutive days a week for six weeks. The patient was told to continue all current medicines. She experienced increased nausea and headache, plus she had rather severe joint pains, as well as increased muscular aches and pains. These symptoms were believed to be due to a Herxheimer type reaction, for they were most bothersome following taking the Metronidazole on Tuesdays and Wednesdays. Moderate relief of these symptoms was obtained by increasing the Prednisone by one tablet on these days.
5/29/84: Condition unchanged, patient complaining of increased nausea from the medication and dialysis. Blood Pressure 140/70; Temperature 98.6; Weight 107#.
6/19/84: Patient complaining of worse nausea, with wretching and more joint stiffness. She doesn’t feel that she is “getting any better”. Blood pressure 140/70, Temperature 98, Weight 106#, Rx – Take Allopurinol 300 mg. 2 times daily for 1 week, and gradually reduce and discontinue Prednisone over the next 3-4 weeks.
7/23/84: Nausea continues, still feels terrible. (Blood pressure 140/74; Temperature 98; weight 104#; Rx – DMSO 5cc in 500 cc D5W [5% Dextrose Solution] Intravenous over 1 hour.)
7/25/84: Less nausea today, but really not feeling any better. Blood Pressure 142/76; Temperature 99; Weight 103#; Rx – DMSO 5cc infusion #2 no problems encountered. 7/27/84-8/17/84: Patient received 5cc DMSO in 500 cc D5W (5% Dextrose Solution) over a 3 hour time span without adverse effects of any sort. Her vital signs remained the same. These infusions were given 3 times weekly.
8/27/84: This date I talked with Dr. Stanley Jacobs, M.D. of the University of Oregon regarding his treatment of scleroderma and rheumatoid arthritis with DMSO. He uses 0.5-1.0 cc of DMSO per kilogram of body weight three times weekly. (The DMSO used was Rimso 50, which is 50% DMSO.) Since this patient had been on only 5 cc DMSO per treatment, it was decided to increase her DMSO by 5-10cc per treatment until her maximum dose of 50 Gm. DMSO in 500cc D5W (5% Dextrose Solution) was reached, and then to continue treatments three times per week at that level. She was given 10cc DMSO today in the infusion, without untoward effects.
9/10/84: Intravenous #19 to day with 32-1/2cc DMSO. Blood Pressure 122/70; Weight 105. Patient appears somewhat improved, as the nausea is mild and intermittent. She seems to be improving and gaining strength weekly. She can now wrinkle her forehead, smile, and walk slowly with assistance. Serum Creatinine 3.9; Serum Creatinine Clearance 13. Kidneys are evidently regaining some function.
9/24/84: 45cc DMSO given today in 23rd treatment. Patient is responding well to therapy, skin is softening, joints are mobile, except for fingers, and she is walking almost normally without assistance. BUN 57; Creatinine 4.2. Liver function studies were normal. Hb 8.9; White Blood Count 7300. Patient told to keep taking Fe script (Iron prescription) for low hemoglobin. I talked with Dr. Thompson at Hermann Hospital. She is pleased with patient’s progress and said we should continue the treatments, and that she would be happy to continue to assist in the care of this patient.
9/26/84: 50cc DMSO given intravenous today without side effect except for the garlic-like odor DMSO gives. The patient continues to improve and feel well. Blood Pressure 122/70; Weight 103#.
10/12/84: Continues improving, offers no complaints. Treatment #29 today. Hemoglobin 8.7; Ca 9.4; BUN 48; Creatinine 3.8; Glucose 88; Triglycerides 391; HDL 44.2; Alkaline Phosphatase 46.9; SGOT 16; LDH 90; P 4.8; Cholesterol 314; Uric Acid 3.8; Na+ 156; K+ 4.7; 24 Hr. Creatinine Clearance 13.1; Urinalysis: Specific Gravity 1.010; pH 6; Rest of Urinalysis negative; Vital Statistics unchanged.
11/27/84: Patient has not had a treatment in one month, so we will go back to 30cc DMSO and go back to 50CC with next infusion. Patient looks great, is walking briskly without any problem, and is free of any discomfort. The skin appears normal and is normal to the touch, having lost its slick, shiney appearance. Hemoglobin 9.6; White Blood Count 6000; Ca 9.2; BUN 51; Creatinine 3.0; Triglycerides 398; Electrolytes and liver tests were normal. Prognosis now looks good.
12/22/84: Dr. Thompson discontinued peritoneal dialysis, but left the catheters in place in the event we have to re-institute dialysis. Patient is improving very well at this time, having a lot of energy, and carries out her normal household duties. Fingers are much more flexible and patient can almost clench fists. She has had 39 DMSO infusions to date. Blood Pressure 140/70; Weight 106#; Serum Creatinine 3.0.
1/21/85: Infusion #44, 35CC DMSO. Blood Pressure 160/ 80; Weight 107#.
1/31/85: Patient complaining of slight headache. Physical exam not remarkable, and I can only explain increase in Blood Pressure by the fact that she hasn’t been getting her treatments very regularly. Blood Pressure 160/102; Weight
105#. She was told to increase Capoten from 75 Mg at bedtime, to 50 Mg. a.m. and 75 Mg. at bedtime; Hemoglobin 11.5; White Blood Count 13,900; Normal Differential Urinalysis negative; BUN 57.1; Creatinine 3.0; Na+ 145; K+ 5.0.
2/26/85: Infusion #49, 35cc DMSO. Patient continues to improve, although lab data remain at December 84 levels. We have started adding 2 cc B6 and 15cc (7.5Gm.) ascorbic acid to each intravenous beginning 2/8/85. No unwanted side effects have been observed.
3/26/85: 30cc DMSO today in treatment #53. Patient is doing very well, offering no complaints. Hemoglobin 10.9; White Blood Count 6000; BUN 68; Creatinine 3.3; Urine output normal; Blood Pressure 130/80 Weight 101#.
4/25/85: Infusion #57, with 50cc DMSO. No problems. Patient seems to continue improving. Blood Pressure 140/84; Weight 102#; BUN 57.2; Serum Creatinine 2.7.
5/30/85: Infusion #65 today. No DMSO, just 1cc EDTA in 500cc D5W, with 2CC B6 and 15cc ascorbic acid given intravenous over 3 hours. No adverse effects noted. Preinfusion Blood Pressure 140/82. Post infusion Blood Pressure 140/80. Hemoglobin 10.6; White Blood Count 5000; 24 Hr. Creatinine Clearance 21.37; Serum Creatinine 2.7.
6/6/85: Infusion #66 with 50cc. DMSO. No Problems. Blood Pressure 140/80; BUN 48; Serum Creatinine 2.8. Skin of face, arms, legs, and hands approaching normal. Patient has lost her Mauskopf appearance, and has normal mobility of the facial skin.
6/10/85: Infusion #67, with 2cc EDTA without problem. Preinfusion Blood Pressure 160/80. Postinfusion Blood Pressure 162/76; Weight 107#. Patient offered no complaints during, or after infusion. BUN 45.8; Creatinine 3.0; 24Hr. Creatinine Clearance 21.37; Urinalysis Specific Gravity 1.010; pH 5.0; Protein trace; 1-2 White Blood Count/high powered field.
6/20/85: Infusion #68, 50CC DMSO and 2CC EDTA. Patient complained of nausea, and had one episode of vomiting during the infusion, which she felt was due to the DMSO. Will reduce DMSO to 40CC next infusion. Preinfusion Blood Pressure 160/90. Postinfusion Blood Pressure 162/88; Weight 105#.
7/11/85: Treatment #70 continued with 40cc DMSO and 2cc EDTA – no complaints or problems. Preinfusion Blood Pressure 150/92. Postinfusion Blood Pressure 15/90; Hemoglobin 11.2; 24 Hr. Creatinine Clearance 23.71. Patient appears and says she feels normal.
7/22/85: EDTA increased to 3cc, along with 40cc DMSO for infusion #72. Preinfusion Blood Pressure 150/90. Postinfusion Blood Pressure 150/86; Weight 105#. Procedure was tolerated well by patient. BUN 58.7; Creatinine 2.6; Urinalysis: Negative.
7/30/85: For infusion #73, EDTA was increased to 5cc, again with 40cc DMSO. No problems encountered during or after treatment. Pre, and post infusion Blood Pressure 150/86; Weight 106#; BUN 55.4; Creatinine 2.8.
8/19/85: Infusion #74 with 5cc EDTA and 40cc DMSO was well tolerated by the patient, and there were no difficulties during or following the treatment. Preinfusion Blood Pressure 142/90, Postinfusion Blood Pressure 140/90; Weight 105#; BUN 45.7; Creatinine 3.0.
10/18/85: Infusions 74 thru 81 were given with 5cc EDTA only and were without incident. Blood Pressure remained in the 150/84 range, and patient continued to progress very well. Her Weight remained the same, but she was having to diet to keep her weight 105# or below. BUN 41; Creatinine 2.7; Creatinine Clearance 21.
11/5/85: Since it had been almost a month from the last treatment, only 20cc DMSO were given in infusion #82. It was without incident. BUN 47.9; Creatinine 2.4; Creatinine Clearance 28.39; Blood Pressure 142/80; Urinalysis: negative; Weight 105#.
12/11/85: Infusion #83 was with 7cc EDTA, 5cc ascorbic acid, and 5cc (1250Mg) Pantothenic Acid all in 50cc D5W (5% Dextrose Solution) intravenous. This was given in 1 hour, there were no adverse effects, lab values and Blood Pressure readings remained the same.
1/6/86: About middle of December 85, Dr. Thompson removed the peritoneal dialysis catheters, since they had not been used for one year.
7/25/86: Since 2/5/86 patient has received infusions 84-90 on the average of one per month, with no adverse effects. All of these treatments contained EDTA 8cc, ascorbic acid 15cc, in 50cc D5W (5% Dextrose Solution), given in one hour. BUN 48; Creatinine 1.6, Creatinine Clearance 38.66. Infusion #91 was given this date. Blood Pressure 150/90; Weight 110#. Patient has felt well and has led a normal life for the past six months.
The patient has not been seen at the Kidney Institute at Hermann Hospital since January 1986 although Dr. Thompson has followed her progress by phone, through my office, and with the patient.
Dr. Ronald Davis expresses his heartfelt gratitude to Dr. Katy Thompson of the Texas Kidney Institute at Hermann Hospital, Houston, TX and to Dr. Stanley Jacobs of the University of Oregon for their kind and able assistance and cooperation in the treatment of this patient.
The following two cases are condensations of and the cases just reported. They came from a presentation given by Ronald Davis, M.D. to a medical convention.
The Reversal of Scleroderma Report of Two Cases
September 6, 1994, by Ronald M. Davis, M.D.
Description: The procedures used for the arresting of the progress of two cases of severe scleroderma and the return of the patients to near normal health and activity. One patient was treated with intravenous EDTA and DMSO and with oral anti-amoebics, the other patient with intravenous EDTA and DMSO, alternating with intravenous H202, and oral anti-amoebics.
Title: The reversal of scleroderma(progressive systemic sclerosis), report of two cases, Davis, RM.
Abstract: This is a report of the reversal of two cases of scleroderma, the first case that of a fifty year old white female with severe kidney involvement, treated with intravenous EDTA and DMSO therapy, and Metranidazole and Allopurinol tablets (according to the Rheumatoid Disease Foundation protocol). The second case is of a fifty-five year old Mexican female with early disease, but having rather severe involvement of the hands, face, and arms. She was treated with a combination of intravenous EDTA & DMSO therapy, alternating with intravenous H202 (0.03%). Metranidazole and Allopurinol tablets were also used with this patient. The response of these patients to the described therapies is outlined in this report. Conventional therapies had failed in both patients.
Scleroderma is among the connective tissue diseases, which include systemic lupus erythematosus, rheumatoid arthritis, polymyositis-dermatomyositis, Sjogrens Syndrome, and mixed connective tissue disease. They are characterized by chronic inflammation, and a dysfunctional immune system, involving joints, serosal membranes, connective tissue and blood vessels in multiple organs (1). Kidneys and lungs are the organs most commonly affected.
The standard treatment for scleroderma consists of large doses of steroids and methotrexate as well as other anti-cancer agents, and gold therapy. These treatments, while at times do offer some relief from the disease, are attendant with unwanted, severe, and sometimes fatal side effects. Death due to the ravages of the disease is the eventual outcome. Although some cases of spontaneous remission have been reported they are very rare.
Case 1:
This first case of scleroderma was a forty-nine year old lady who had been told by her rheumatologist at the Houston Medical Center, that there was nothing more he could do for her. The patient was terminally ill and she wanted to take our therapy, as she had been given no hope of recovery.The patient first began to notice a sensation of swelling and tightness of the skin, face, and extremities approximately two years prior to being seen in our office May 22,1984. These symptoms rapidly progressed to the point of rendering the patient unable to walk, or do daily household work. Evidently her kidneys had become affected early in the disease, as hypertension and headache were early symptoms. The patient had been on antihypertension medication for over one year, and on peritoneal dialysis for nearly nine months, before being seen in our office. She was under the care of a rheumatologist in Houston, and the Texas Kidney Institute at Hermann Hospital in Houston.
Medications being taken as of May 22, 1984:
- Dialome - 1 t.i.d.
- Compazine -25 Mg. tabs i. q.i.d. for nausea.
- Capoten - 75 Mg. i. b.i.d.
- Prednisone - 5 Mg i. daily.
- Catapres - o.1 Mg 1 @ hs.
- Peritoneal dialysis with 1 liter of solution(prepared by The Texas Kidney Institute at Hermann Hospital) in Houston.
Physical Examination:
BP 140/90 P 94 T 100/O R 20 Ht 60" Wt 109#
The patients’ skin was white and glistening, and appeared to have been stretched tightly over the bony skeleton. The joints at the elbows, wrists, knees, and ankles very difficult to move. The fingers were fixed in flexion and could not be moved at all. She had the classic Mauskopf face.
Initial Laboratory Data:
Hgb. WBC Ca++ BUN Creat. Gluc. Trig. Uric A. SGOT SGPT Prot. Alb.
8.4 7400 9.3 91 8.3 113 377 6.6 28 23 7.0 3.7 Glob. LDH Phos. 24hr Creat Cl. Na+ K+ Cl- Co2
3.3 204 4.6 7.0 140 5.0 100 24 Urinalysis: S.G.1.010 Ph 5.0 Prot. 1+ Gluc. - Casts 2+rbc Bact.
1+ rbc 4-5/hpf wbc 3-4/hpf.
Chest X-ray: Negative
EKG: Sinus tachycardia, otherwise normal.
Impression: Progressive Systemic Sclerosis (Scleroderma)
Nephrosclerosis with kidney failure secondary to scleroderm. Severe Anemia secondary to the two conditions above
Treatment Plan:
- Anti-Amoebic therapy
- I.V DMSO therapy
- I.V. Chelation therapy
- Physical therapy as tolerated by the patient
Clinical course: On May 22, 1984 anti-amoebic therapy was initiated in accordance with The Rheumatoid Disease Foundation protocol, which is as follows; Zyloprim 300 Mg t.i.d. for 7 days. Flagyl 500 Mg - two tablets A.M. and P.M. on two consecutive days a week for six weeks(2). The patient was told to continue all current medications. She experienced increased nausea and headache, plus she had severe joint pains as well as increased muscular aches and pains. These symptoms were thought to be due to a Herxheimer type reaction, for they were most bothersome following taking the Flagyl on Tuesdays and Wednesdays.
On 7/27/84 the patient received an IV of 5cc of Rimso 50 (50% DMSO) in 500cc D5W over 3 hr. timespan, without untoward effects(3). These infusions were continued three times weekly, increasing the Rimso 50 by 10cc per treatment until the maximum dose of 50cc of Rimso 50 was reached. This dosage was decided uponfollowing a telephone conversation with Dr. Stanley Jacob of the University of Oregon, this being his protocol for the treatment of scleroderma (8/27/84).
By the fourth month of therapy, the Prednisone had been gradually withdrawn and discontinued, kidneys regaining function and patient able to walk without assistance. Seven months after the initiation of therapy, enough kidney function had returned to allow stopping dialysis. The patient was feeling well and appeared well in all respects. She still had some restriction of motion of the fingers, but was improving steadily, and skin had lost its shiny slick look.
One year after beginning therapy, the patient’s condition had improved to the point that it was felt we could begin adding EDTA to the infusions. This was done 5/30/85, at which time 1cc of EDTA was added to the iv as was 15cc ascorbic acid, and 2cc B-6, and given over three hours. No side effects were noted. Pts. Creat. was 2.8, her clearance was 21.7.
The EDTA was gradually increased to 8cc as the patients kidney function continued to improve. She continued improving on treatments monthly until she pronounced herself “cured” on 10/1/87. She has been on only otwo medications since that time, those medicines being Capoten 75Mg i. daily and Catapres 0.1 Mg @ Hs. The patient is leading an active, normal life.
Case 2:
This fifty-five year old Mexican lady presented with tightness and swelling of face, hands, arms and feet. Her symptoms began approximately one year prior to coming to our office. She had had surgery on the right wrist for carpal tunnel syndrome in December 1990. She was supposed to have the other wrist operated on too, but since she did not improve after the first surgery, it was decided not to operate on the other wrist. She was being treated at Lyndon B. Johnson Hospital in Houston, Texas.
Medications being taken 8/12/91:
- Acetaminophen w/codeine #3 2 tabs q 4-6 hrs. prn pain.
- Tylenol 5oo Mg. 1 tab q 4 hrs.
- Pen V-K tabs 250Mg. 1 tab q 6 hrs.
- Cephalexin 250 Mg. caps 1 capsule q 6 hrs.
- Procardia caps, 10Mg. 1 capsule t.i.d.
- Hydroxyzine 250Mg. tabs 1 tab q 4-6 hrs. prn itching.
- Cuprimine 250Mg. caps 1 cap b.i.d.
- Ibuprofen 400Mg. caps 1 tab t.i.d.
- Flexeril 10Mg. tabs 1 tab b.i.d.
- Tagamet 300Mg. tabs 1 tab q.i.d.
- Zantac 150Mg. tabs 1 tab b.i.d.
Physical Exam:
BP 120/80 P 74 T 99 R 16 Ht. 62" Wt. 178#
Physical findings were limited to the skin and joints. There was difficulty moving the hands and fingers. The fingers were fixed in a mild degree of flexion and patient was unable to close her fists. The skin of the hands and arms, to the mid humerus level was darkened and very firm and painful to the touch. The feet and toes were similar to the hands, as the toes could not be moved, and were edematous. The patient’s skin of the feet and legs to her knees was of a darkened color similar to the arms. The skin of arms and legs had a glistening, shiny, slick appearance.
Laboratory Data: Done at LBJ Hosp. 8/12/91
Pulmonary function study was normal.
Blood studies, serum electrolytes, smac 28 were wnl.
Hgb 11.8 Hct 35.6 ESR 50 RA neg ANA Pos 1:320 Speckled pattern
Sjogren Antibodies A and B negative
Scleroderma antibodies Pos 1:640
X-rays Barium swallow negative Chest X-ray Mild cardiomegaly.
EKG Not done
Impression:
- Progressive Systemic Sclerosis (Scleroderma).
- Carpal Tunnel Syndrome, secondary to scleroderma,(operated);
- Anemia, mild, secondary to 1
- Possible mild asymptomatic cardiomyopathy secondary to 1.
Treatment Plan:
- Anti-Amoebic therapy
- I.V. Chelation-Dmso Therapy.
- I.V. Hydrogen Peroxide Therapy.
- Physical Therapy as tolerated by the patient.
- MSM p.o. q.id.
Clinical Course: The anti-amoebic therapy was started on 8/14/91. Moderate Herxheimer reaction was noted on the first two episodes of taking the medication, but was hardly noticeable the next four treatment episodes. At the same time, iv infusions of chelation-DMSO were started and continued three times weekly. There was gradual but quite evident improvement in the patients condition over the next year. In September 1992, iv H202 was started three times weekly instead of the chelation-DMSO infusions. 2.5cc of 3% H202 in 250cc D5W, with 1.6cc NaHCO3 was the formula used in the treatment(4). This was a 0.03% solution of H202 .
The response to this therapy was immediate and dramatic, as the patient began to have softening of the tissues of the hands, arms, feet, and legs almost within the first week of treatment. She stated that the peroxide treatment made her “itch on the inside” of her hands, arms and feet, but the next day after the infusion she felt a lot better. She felt that the peroxide infusions were giving much better results than the chelation-Dmso infusions. Her condition continued to improve with each infusion and between infusions, even when she went 2-3 months between treatments. She has had a total of 80 chelation-DMSO infusions and 30 H202 infusions, and her condition is continuing to improve. The skin of her face, arms, hands, legs, and feet is normal in appearance and texture. She no longer has fatigue and malaise, and her energy and activity levels are normal. She has normal function of her hands and fingers, and is without pain.
Discussion: There seemed to be a better response of the second patient to H202 therapy than the chelation-DMSO therapy. It is difficult to compare the two cases, for the lady in case 1 was more acutely ill with systemic disease, which the lady in case 2 did not have, however their overall responses to treatment was excellent, albeit quite different. It was the patient in case two’s opinion, and my opinion that the H202 infusions were superior to the Chelation-DMSO infusions. I shall continue to use both therapies, but will begin with H202 infusions, as well as the anti-amoebic therapy in the future.
References for Part 1
- Textbook of Internal Medicine, J.B. Lippincott Company, East Washington Square, Philadelphia, PA 19105, 1989.
- The Merck Manual of Diagnosis and Therapy, 13th Edition, Merck, Sharp & Dohme Research Laboratories, Division of Merck & Co., Inc., Rahway, N.J.
- Burton Goldberg Group, Alternative Medicine: The Definitive Guide, Future Medicine Publishing Co., Puyallup, WA, 1994.
- Ronald Davis, M.D., "A Treatment for Scleroderma & Lupus Erythematosus," Supplement to The Art of Getting Well, The Arthritis Trust of America/The Rheumatoid Disease Foundation, 7376 Walker Road, Fairview, TN 37062, 1989; also Permission to republish portions granted toTownsend Letter for Doctors, 911 Tyler Street, Port Townsend, WA 98368, December, 1989, p. 625.
- Physicians' Desk Reference, Medical Economics Co., Inc., Oradell, N.J. 07649, 1989.
- Efrain Olszewer, M.D.,Fuad C. Sabbag, M.D., Alan Rory Zapata, M.D., DMSO (Dimethylsulfoxide) Treatments in Arthritis, Supplement to The Art of Getting Well, The Arthritis Fund/The Rheumatoid Disease Foundation, 5106 Old Harding Road, Franklin, TN 37064; also see Pat McGrady, Sr., The Persecuted Drug: The Story of DMSO, The Nutri-Books Corporation, Box 5793, Denver, CO 80217, 1981; Mildred Miller, A Little Dab Will Do Ya! DMSO: The Drug of the 80's, Quality Advertising Co., Degenerative Disease Medical Center, Las Vegas, NV, 1981.
- Anthony di Fabio, "Chelation Therapy," Supplement to The Art of Getting Well, The Arthritis Trust of America/The Rheumatoid Disease Foundation, 7376 Walker Road, Fairview, TN 37062, 1993.
- Dr. Paul K. Pybus, The Herxheimer Effect, Supplement to The Art of Getting Well, The Arthritis Fund/The Rheumatoid Disease Foundation, 5106 Old Harding Road, Franklin, TN 37064, 1991.
- Charles Farr, M.D., Ph.D., "Hydrogen Peroxide Therapy," Supplement to the Art of Getting Well, The Arthritis Trust of America/The Rheumatoid Disease Foundation, 7376 Walker Road, Fairview, TN 37062, 1992.
- 10. Personal letter from Richard A. Kunin, M.D.
- Alan R. Gaby, Townsend Letter for Doctors, August/ September 1995.
- Dr. Tsue-Tsair Chi, N.M.D., Ph.D., Mineral Infrared Therapy, Chi's Enterprises, Inc., 5465 E. Estate Ridge Rd., Anaheim, CA 92807, 1933.
- Personal communication with Rex E. Newnham, D.O., N.D., Ph.D. November 6, 1995.
- A.V. Constantini, M.D., The Fungal/Mycotoxin Connections: Autoimmune Diseases, Malignanacies, Atherosclerosis, Hyperlipidemias, and Gout, Keynote Speaker, American Academy of Environmental Medicine, Reno, Nevada, 1993.
- Personal interview with Gus J. Prosch, Jr., M.D., November 22, 1995.
- Jwing-Ming Yang, Arthritis -- The Chinese Way of Healing and Prevention, YMAA Publication Center, Yang's Martial Arts Association (YMAA), 38 Hyde Park Avenue, Jamaica Plain, Massachusetts 02130, 1991.
- Alan R. Gaby, M.D., "Commentary," also Jonathan V. Wright, M.D., "Treatment of Lupus."Nutrition and Healing, C/O Publishers Mgt. Corp., PO Box 84909, Phoenix, Arizona 84909, Volume 2, Issue 12, December 1995.
- 18. Personal communication with Paul A. Goldberg, M.P.H., D.C.
- Personal interview with Roger Jahnke, O.M.D.
- Personal correspondence with Ronald M. Davis, M.D.
- Personal interview with Dr. Catherine Russell.
- H. Hugh fudenberg, Giancarlo Pizza, "Transfer Factor 1993: New Frontiers," Progress in Drug Research, Vol. 42, Birkhauser Verlag Basel (Switzerland), 1994.
- Joel Fuhrman, M.D., "Fasting and Detoxification," Townsend Letter for Doctors & Patients, April 1996, p. 84.
References for Part 2
- Textbook of Internal Medicine, J.B. Lippincott Company, East Washington Square, Philadelphia, PA 19105, 1989.
- The Merck Manual of Diagnosis and Therapy, 16th Edition, Merck, Sharp & Dohme Research Laboratories, Division of Merck & Co., Inc., Rahway, N.J, 1992.
- Burton Goldberg Group, Alternative Medicine: The Definitive Guide, Future Medicine Publishing Co., Puyallup, WA, 1994, 2002.
- Ronald Davis, M.D., "A Treatment for Scleroderma & Lupus Erythematosus," Supplement to The Art of Getting Well, The Arthritis Fund/The Rheumatoid Disease Foundation, 7376 Walker Road, Fairview, TN,1989; also permission to republish portions granted toTownsend Letter for Doctors, 911 Tyler Street, Port Townsend, WA 98368, December, 1989, p. 625.
- Efrain Olszewer, M.D., Fuad C. Sabbag, M.D., Alan Rory Zapata, M.D., DMSO (Dimethylsulfoxide) Treatments in Arthritis, Supplement to The Art of Getting Well, The Arthritis Fund/The Rheumatoid Disease Foundation,7376 Walker Road, Fairview, TN 37062; also see Pat McGrady, Sr., The Persecuted Drug: The Story of DMSO, The Nutri-Books Corporation, Box 5793, Denver, CO 80217, 1981; Mildred Miller, A Little Dab Will Do Ya! DMSO: The Drug of the 80's, Quality Advertising Co., Degenerative Disease Medical Center, Las Vegas, NV, 1981.
- Anthony di Fabio, "Chelation Therapy," Supplement to The Art of Getting Well, The Arthritis Trust of America/The Rheumatoid Disease Foundation, 7376 Walker Road, Fairview, TN 37062, 1993.
- Dr. Paul K. Pybus, "The Herxheimer Effect," Supplement to The Art of Getting Well, The Arthritis Trust of America/The Rheumatoid Disease Foundation, 7376 Walker Road, Fairview, TN 37062, 1991.
- Charles Farr, M.D., Ph.D., "Hydrogen Peroxide Therapy," Supplement to The Art of Getting Well, The Arthritis Trust of America/The Rheumatoid Disease Foundation, 7376 Walker Road, Fairview, TN 37062, 1992.
- Physicians' Desk Reference, Medical Economics Company, Inc., Oradell, NJ 07649.
- Dr. Tsu-Tsair Chi, N.M.D., Ph.D., Mineral Infrared Therapy, Chi's Enterprises, Inc., 5465 E. Estate Ridge Rd., Anaheim, CA 92807, 1993.
- Personal communication with Rex E. Newnham, D.O., N.D., Ph.D. November 6, 1995.
- A.V. Constantini, M.D., The Fungal/Mycotoxin Connections: Autoimmune Diseases, Malignanacies, Atherosclerosis, Hyperlipidemias, and Gout, Keynote Speaker, American Academy of Environmental Medicine, Reno, Nevada, 1993.
- Jwing-Ming Yang, Arthritis -- The Chinese Way of Healing and Prevention, YMAA Publication Center, Yang's Martial Arts Association (YMAA), 38 Hyde Park Avenue, Jamaica Plain, Massachusetts 02130, 1991.
- Gotu Kola (Centella asiatica) for Scleroderma, The American Journal of Natural Medicine, Vol. 2, No. 9, IMPAKT Communications, Inc., November 1995, p. 16; from Sasaki S., et. al: Studies on the mechanism of action of asiaticoside (Madecassol) on experimental granualtation tissue and cultured fibroblasts and its clinical application in systemic scleroderma. Acta Diabetologica Latina 52:141-50, 1972.
- Personal interview with Mark Davidson, D.O., N.D.; also see "Wellness: Why You Need Detoxification and Nutritional Support," Alternative Medical Digest, Issue 8, Future Medicine Publishing, Inc., Puyallup, Washington 98371.
- Julian Whitaker, M.D., "DMSO Update," Health & Healing, Phillips Publishing, Inc., 7811 Montrose road, Potomac, MD 20854, December 1955.
- Personal interview with Roger Jahnke, O.M.D.
- Correspondence with Ronald M. Davis, M.D.
- Personal interview with Dr. Catherine Russell.
- H. Hugh fudenberg, Giancarlo Pizza, "Transfer Factor 1993: New Frontiers," Progress in Drug Research, Vol. 42, Birkhauser Verlag Basel (Switzerland), 1994.
References for Part 3
- Mukerji Baasanti, Alpert Martin A. Hardin Joe G When the lungs are involved by connective tissue disease. Postgraduate Medicine 1993;94(5):147
- di Fabio, Anthony, Rheumatoid Diseases Cured At Last, Franklin TN,1982, The Arthritis Trust of America/The Rheumatoid Disease Foundation, 7376 Walker Road, Fairview, TN 37062;
- Halstead BW, Youngberg S. The DMSO Handbook Colton CA 1981 Golden Quill Publishers Inc. P.O Box 1278 Colton CA
- Farr CH Workbook on Free Radical Chemistry and Hydrogen Peroxide Metabolism including protocol for the intravenous administration of hydrogen peroxide Oklahoma City OK 1989 IBOM Foundation P.O. Box 891954 Oklahoma City, OK 73189
- Cranton EM, Bypassing Bypass Medex Publishers Inc. Ripshin Rd., P.O. Box 44 Troutdale VA 24378-0044 1982
- Halstead BW The Scientific Basis of Chelation Therapy, Colton, CA 1979 Golden Quill Publishers Inc. P.O. Box 1278 Colton CA 92324
- Cranton EM A Textbook on EDTA Chelation Therapy J of Adv Med 2(1/2) 1989
- Douglas WC Hydrogen Peroxide MEDICAL MIRACLE Atlanta GA 1992 Second Opinion Publishing P.O. Box 467939 Atlanta GA 30346-7939
Acknowledgements
Stanley W. Jacob, M.D., Oregon Health Sciences Univ. Portland, Oregon who saw the patient in case 1 in consultation in July 1984, and for his assistance via telephone conversations regarding his DMSO protocol.
Charles H. Farr M.D., Ph.D., for the many interruptions in his busy schedule, to assist in the care of both of the patients, with answering questions about protocols of EDTA, DMSO, and H202 therapies.
Garry Gordon, M.D., without whose help I would probably not have gotten involved in chelation and other alternative therapies.
Katy Thompson, M.D., Texas Kidney Institute, Hermann Hospital, Houston, Texas for her kind assistance and co-operation in the care of the patient in case 1.
Sources are given in references. Authors of contributions\quotations are alphabetically arranged; major author, if any, is in bold.
- Jack Blount, M.D.
- Ronald Davis, M.D.
- Stanley Jacobs, M.D.
- Dr. Katy Thompson
- Responsible editor/writer: Anthony di Fabio
Copyright 1989, 1997. All rights reserved by the The Roger Wyburn-Mason and Jack M. Blount Foundation for Eradication of Rheumatoid Disease AKA The Arthritis Trust of America.®
The Rheumatoid Disease Foundation / The Arthritis Trust of America was dissolved in 2020 and all website content was transferred to the Foundation for Alternative and Integrative Medicine.


