StrophanthusGratusSingleBlossom.jpg

Photo by Richard Foo TH, ©2015 / CC BY-NC-ND 2.0
Strophanthin comes from an extract of an African plant called strophanthus gratus. Dr. Berthold Kern says the regular, clinical use of oral g-strophathin prevents lethal myocardial tissue acidosis and substantially reduces the incidence of myocardial infarction and completely prevents infarction deaths.
Coronary artery disease is currently the leading cause of death in the United States. Despite the increasing sophistication of surgical techniques, the introduction of new techniques such as balloon angioplasty, and a number of new drugs (e.g. beta blockers, calcium antagonists), it is estimated that over 1 million heart attacks will occur this year, resulting in 500,000 deaths. In short, we do not have an adequate therapeutic solution to the problem of myocardial infarction (heart attack).
The cornerstone of therapy for treatment and prevention of myocardial infarction is to remove blockages in coronary arteries that are thought to be the cause of the infarction. This adheres to the widely accepted coronary artery thrombosis theory of infarction; that is, arteries become clogged with plaque, damaged from such things as smoking or high cholesterol. A clot forms a fissure in the plaque. The clot may shut off the blood flow of the coronary artery, causing a heart attack. It is deceptively simple: The coronary arteries are clogged. No blood can flow, so the muscles of the heart cannot be supported, and heart metabolism stops, leading to death.
bertholdkern.jpg
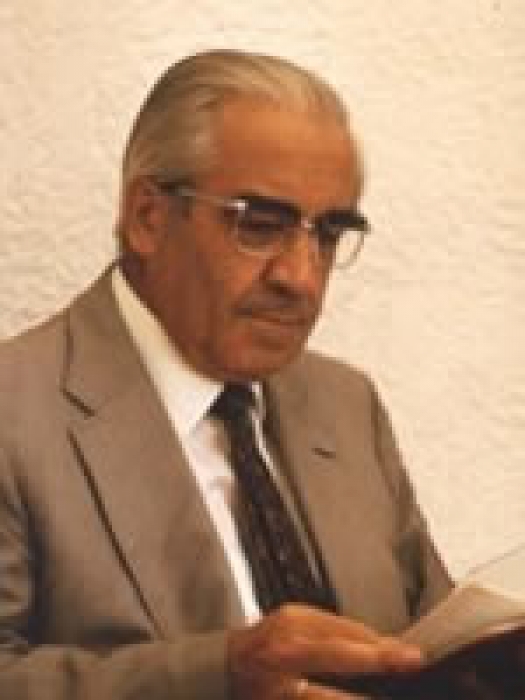
Berthold Kern, MD
In Germany, another theory of myocardial infarction has been proposed by Dr. Berthold Kern (1911-1995). Dr. Kern, while performing autopsies in Germany in the 1930s and 1940s, observed that the findings of these autopsies did not corroborate the coronary obstruction hypothesis. He began researching the literature, looking for clues as to an alternative etiology. What he found was not only a new theory that may provide the missing piece of the coronary obstruction theory, but a therapy now being used by over 5,000 physicians in Germany with reportedly remarkable success.
Dr. Kern's claims, as set forth in his 1971 informational paper, Three Ways to Cardiac Infarction, can be summarized as follows:
- The coronary obstruction theory cannot adequately explain observed facts.
- The major etiologic factor underlying myocardial infarction is a primary chemical destructive process, cause by unchecked metabolic acidosis (accumulation of acid) in the left ventricular tissue and substantially unrelated to coronary artery disease.
- The regular, clinical use of oral g-strophathin (a cardiac glycoside derived from the West African plant strophanthus gratus):
- Prevents lethal myocardial tissue acidosis, and thereby
- Substantially reduces the incidence of myocardial infarction and completely prevents infarction deaths.
Dr. Kern's observations that most myocardial infarctions occur in patients without significant obstruction of the coronary artery supplying the infracted tissue finds great support in the American peer-reviewed literature. Since 1948, over a dozen reports of post-mortem examination of infracted hearts have consistently failed to corroborate the coronary artery thrombosis theory of myocardial infarction. That is, victims of fatal heart attacks have had no evidence whatsoever of coronary occlusion.
An example of the degree of non-confirmation can be ascertained by the following quote from a 1980 article on Circulation:
"These data support the concept that an occlusive coronary thrombus has no primary role in the pathogenesis of a myocardial infarct."
The reviewer went on to note,
"These reports also present clear refutation of the most common explanation used today to dismiss autopsy findings which detect no coronary thrombi, i.e. that thrombi existed at infarction but have since lysed, embolized or washed away."
There does not appear to be any literature that effectively refutes these autopsy findings.
Another source of inconsistent data are the many reports in the literature of myocardial infarction in patients without coronary artery disease, as deduced by normal coronary angiograms. Other autopsy data has revealed widely scattered areas of necrotic tissue that produces a substantial incongruence between the area of infarction and the arterial supply.
In a 1988 editorial published in the New England Journal of Medicine titled "Twenty years of coronary bypass surgery," Thomas Killip observed that
"Neither the VA [Veterans' Administration] nor CASS [the National Institute of Health's Coronary Artery Surgery Study] has detected a significant difference in long-term survival between the two assigned treatment groups [surgical vs. medical] when all patients have been included…"
More recent work with coronary angioplasty and anti-thrombolytic agents has also failed to demonstrate any clear cut improvements in survival.
Dr. Kern went a step further. In his review of the literature, he came across the notion of collaterals (or anastomoses), a finely-meshed network of small blood vessels that act as natural bypass channels in the heart muscle. These collaterals have been made visible by Professor Giorgio Baroldi in studies at the Armed Forces Institute of Pathology.
Baroldi developed a technique for filling the arteries of the heart with artificial blood, a chemical substance that thickens in the blood vessels. When later the tissues were dissolved in acid, the entire structure of blood vessels in the heart was revealed. Kern hypothesized that bypass grafts were created naturally by the body via the collaterals whenever a coronary artery became blocked. Therefore, heart bypass would be redundant to a large degree.
A study by Rentrop et al in the April 1, 1988 issue of The American Journal of Cardiology has produced results completely at odds with the coronary artery blockage theory, and consistent with Kern's hypothesis. In an accompanying editorial, Dr. Stephen Epstein of the National Heart, Lung and Blood Institute summarizes Rentrop and colleagues' "extremely important observations." They found that in an advanced state of the narrowing of the coronary arteries, the supply of blood to the heart muscles is fully assured via collaterals that enlarge naturally in response to the blockage. Interestingly, they observed that the more the coronaries narrow, the less danger there is of heart infarction.
Dr. Kern's second claim, i.e. his proposed new theory of metabolic acidosis, can be summarized as follows: Metabolic conditions in the most healthy of hearts are, at best, marginal in the constantly beating left ventricle. This is the part of the heart responsible for pumping blood to most of the body, the right ventricle merely supplying the lungs. Oxygen and energy requirements are always perilously close to available supplies, and any of the several stressors may cause an oxygen/energy deficit, with deterioration in oxidative metabolism, and consequent development of acidosis. Lack of oxygen sets off the process of zymosis or fermentation metabolism, an anaerobic process, in order to produce energy in the cells. This, in turn, lowers the pH.
This lowering of the pH sets off a destructive chemical process, literally a suicide reaction of the cell. Lysozymal enzymes are released, causing cell self-digestion. This starts as a single point in the muscle, then many points, which eventually join to form a small area of necrotic tissue. Finally, a critical mass is reached, no bigger than the head of a pin, which triggers larger and larger areas of damaged tissue, resulting in infarction (heart attack).
Ideally then, the remedy to address infarction would be a restoration of pH balance to the heart muscle, thereby preventing tissue damage and fatal infarction. The problem Kern faced was how to accomplish this without causing positive inotropy [increasing the strength of the muscular contraction], i.e. without putting further stress on the contracting heart muscle itself. The cardiac glycosides, including digitalis and the strophanthin byproduct known as ouabain, are known to produce such a deleterious effect, and this is why they are not effective against infarction.
This is where Kern made an important re-discovery. In reviewing the literature, he came across the work of Dr. Edens, who in the 1920s had reported on a qualitatively different effect of strophanthin given intravenously versus orally. Specifically, the positive inotropic effects [that is, increasing contraction] that accompanied intravenous administration were not observed with oral administration.
This important observation has been confirmed in a study by Belz published in the European Journal of Clinical Pharmacology in 1984. Utilizing a randomized, placebo-controlled, double blind methodology, the researchers found that the intravenous ouabain (strophanthin) produced the expected increase in cardiac inotropy. However, the investigators stated quite definitely that,
"...the single sublingual (oral) dose of ouabain did not exert a positive inotropic effect."
The postulated mechanism of action, based on animal research done by Adams, Powell and Erdmann, is that there are two receptors in the heart: "High affinity" and "Low affinity." It is thought that intravenous administration triggers low affinity receptors, and thus positive inotropy. High affinity receptors, on the other hand, react to small concentrations of g-strophanthin via oral administration, thereby avoiding the dangerous effect of positive inotropy.
Dr. Kern reported results of his clinical practice in Stuttgart over the period 1947-1968 involving over 15,000 patients. His patients treated with oral g-strophanthin experienced no fatal infarcts and only 20 non-fatal heart infarcts. These patients included many suffering infarction prior to entering the study. In contrast with these results, government statistics for the same time period would have predicted over 120 fatal heart attacks and over 400 non-fatal infarctions in a group of patients this size.
Currently, there are approximately 5000 M.D.s in Germany using and prescribing oral g-strophanthin. The booklet Eine Dokumentation ambulanz-kardiologischer Therapie Ergebnisse nach Anwendung oralen g-strophanthin represents the results of a survey wherein 3645 medical doctors made statements on use of this remedy in their practices from 1976 to 1983. Of these, 3552 gave exclusively positive testimony with no reservations. No one gave a negative response.
In addition to accumulating clinical experience, a number of studies have demonstrated excellent results with oral g-strophanthin. One fascinating report in a real-life setting took place at a German coal mine. During the period 1972-1974, miners suffered episodes of acute chest pain 229 times. Medical help was a two-hour ride away, and 11 miners died during this period. From 1975-1980, all miners who experienced acute chest pain (280 episodes) were immediately given oral g-strophanthin. During this period, which was twice as long as the comparison period, no miners died after the onset of symptoms. No toxic side effects were observed. Many variables were studied, i.e. age better access to treatment, different working conditions, etc to ensure comparability of observation periods.
A rigorous, double blind, randomized control study of oral g-strophanthin in the treatment of angina showed impressive results at statistically different levels. After fourteen days, 81% of patients in the treated group experienced a reduction in attacks, while in the control group, 72% receiving placebos registered an increase in attacks.
In a study of 150 seriously ill heart patients, who altogether had 254 heart attacks, oral g-strophanthin was successful in 85% of the cases. Dr. Dohrmann, who conducted the study, observed,
"A positive result was registered when the severe heart attack abated at least five minutes after the g-strophanthin capsule was bitten through, and after ten minutes at the latest, they disappeared completely."
A consistent feature of clinical reports using oral g-strophanthin is the absence of side effects. The cost of this remedy, which is currently available to German physicians and their patients, is approximately $30 per month for typical use.
At this point, every indication suggests that oral g-strophanthin may be a significant breakthrough in the treatment and prevention of myocardial infarction. What is needed is a definitive American clinical trial.
At an annual meeting of the American College of Cardiology in New Orleans, it was mentioned that every year one million US citizens suffer a heart attack. Of these, about 60 percent get to the hospital alive. About 16 percent never leave the hospital, and a further 10 percent die within a year. This should be keen motivation for a complete and intensive investigation of the benefits of g-strophanthin.
The prospect of replacing heart bypass surgery with a safer, more effective, and less expensive treatment may be another reason to interest other parties in funding American research on oral g-strophanthin.
Visit the World Research Foundation website for more articles on Alternative Therapies.
From the World Research Foundation. Used with permission.

