ArtAssistCompressionSequence.jpg
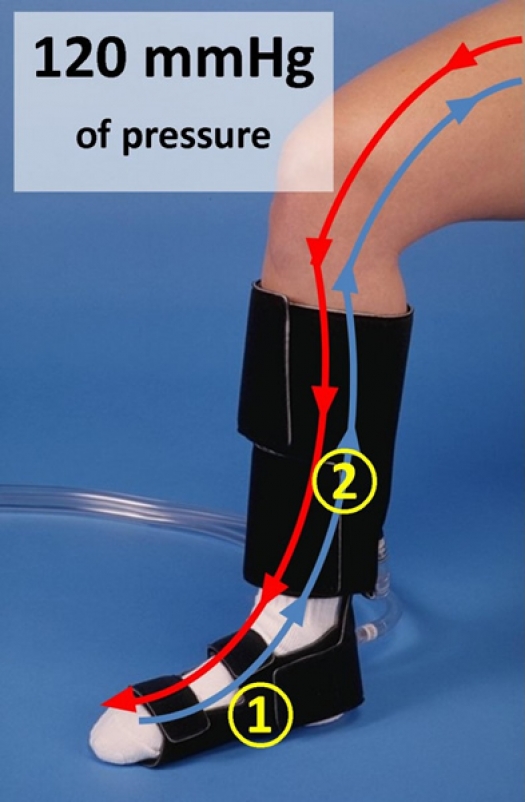
Image and description courtesy of ACI Medical, LLC
The ArtAssist® device compresses the foot and ankle (1).
One second later, the calf is compressed (2).
As a result, the foot, ankle and calf veins are almost completely emptied (blue line).
In return, the arterial blood is more easily pushed down to the toes and blood-deprived tissues (red lline).
Because of this mechanism, blood flow to the skin of the feet can be tripled.
Walking has been shown to have many unexpected health benefits, such as improving cognitive function of the brain, maintaining bone density, alleviating symptoms of depression and improving fitness, but for many people the ability to walk and benefit from these natural effects is severely diminished by existing arthritis, weight-problems, previous amputation, balance problems, advanced age and medical conditions.
Simulation of walking, without the work of muscle-contraction or fall-risk, can be achieved with a non-invasive home treatment, which uses external squeezing of the leg muscles. This will increase blood return to the heart. Studies with ultrasound and laser-technology have demonstrated an immediate increase in the blood flow to the foot as a result of this compression therapy. Application of this massage-effect as the main management for patients with diabetes and non-reconstructable arterial disease has recently demonstrated remarkable results. Because healthcare providers are paid much more for invasive procedures, our healthcare system currently favors costly procedures as the primary solution for circulation problems. In Ireland, a study on 171 patients treated with the compression device, found a savings of about 1.5 million Euros compared to cost of amputation for a matched group of patients. The quality of life was better for patients, who avoided amputation by using the device. The limb salvage rate in the group who used the device was 94% after 3.5 years in this peer-reviewed study, which was published in 20111.
Historical notes/background
In the 19th century, massage therapy of the leg, which mimics the effects of walking, was a widely accepted treatment for poor arterial circulation. As early as 1835, a device to change the pressure around a limb was described2. The earliest devices applied a continuous vacuum on the leg to create a suction effect and allow more blood flow towards the skin. By 1934, the method had evolved into a rhythmical alternation of positive and negative pressures and was called ”passive vascular exercise”3. In 1948 and 1959, various authors4,5 described physiological effects of inflating pneumatic cuffs around a limb in healthy volunteers, but use of a generic edema pump with the stated goal to increase arterial circulation in patients was not mentioned until 19656. Due to its slow inflation and deflation properties, this device did not prove to be effective. Various attempts were made to synchronize the limb-compression to the patients’ heartbeat and between 1980 and 1992 multiple case series7,8 with clinical successes were published. The advent of real-time ultrasound allowed more detailed study of the duration of the flow increase after compression9 and this led directly to the development of the first dedicated arterial assist device (named ArtAssist®) by 1997.
How does it work?
There are several different underlying mechanisms that make the compression method work:
- Mechanical: The driving force for blood to flow through the vessels in the muscles and skin, is the difference in pressure between arteries and veins. The compression decreases the pressure in the veins and thereby increases the pressure difference, which increases flow.
- Release of nitric oxide: The increased friction between the blood and the inner lining of blood vessels (endothelium) results in the production of nitric oxide (endothelium derived relaxing factor) by the inner lining. This has been proven to relax the underlying muscle cells, which opens up the blood vessel and in turn increases the flow.
- Long-term effect: Repeated periods of increased blood flow, triggered by the device, act the same way as training does by increasing the size of small arteries in the muscles (arteriogenesis or collateral formation).
References
Randomized studies and other peer-reviewed papers are cited in the paragraphs by Dr. Kavros. The literature list below is not intended to be comprehensive, but illustrates that throughout time, highly respected journals have contributed:
- Sultan S, Hamada N, Soylu E, Fahy A, Hynes N, Tawfick W: Sequential compression biomechanical device in patients with critical limb ischemia and nonreconstructable peripheral vascular disease. J Vasc Surg 2011;54:440-7
- Murray J: On the local and general influence on the body of increased and diminished atmospheric pressure. Lancet 1835;1:909.
- Hermann LG, Reid MR: The conservative treatment of arteriosclerotic peripheral vascular diseases. Ann Surg 1934;100:750-60.
- Halperin MH, Friedland CK, Wilkins: The effect of local compression upon blood flow in the extremities of man. Am Heart J 1948;35:221-237.
- Loane RA: Effect of rhythmically inflating a pneumatic cuff at the ankle on blood flow in the foot. J Appl Physiol 1959;14:411
- Henry JP, Winsor T: Compensation of arterial insufficiency by augmenting the circulation with intermittent compression of the limbs. Am Heart J 1965;70:79-88.
- Dillon RS: Effect of therapy with the pneumatic end-diastolic compression boot on peripheral vascular test and on the clinical course of peripheral vascular disease. Angiology 1980;31:614-38.
- Steinberg J: Cardiosynchronous limb compression: effects on noninvasive vascular tests and clinical course of the ischemic limb. Angiology 1992;43:453-461.
- van Bemmelen PS, Mattos MA, Faught WE, Barkmeier LD, Hodgson KJ, Ramsey DE, Sumner DS: Augmentation of bloodflow in limbs with occlusive arterial disease by intermittent calf compression. J Vasc Surg 1994;19:1052 8.


