HumanKidneyHealthConditions.jpg
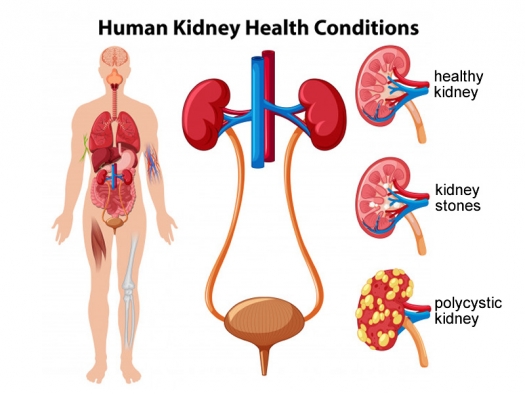
Illustration by brgfx / Freepik.com
The kidneys may well be the most misunderstood of all the major organs. Patients often fail to grasp the seriousness of their condition and, without a proper understanding, cannot take appropriate steps to ameliorate their condition. Part of the reason for this is the very nature of kidney disease. Most of the damage of kidney disease has already taken place by the time the patient becomes aware that there is a problem. The “silent killer” is easy to ignore; and by the time some patients are roused into action, it is in a last-ditch effort to avoid dialysis.
When attempting to properly treat kidney disease, patients usually first look to their nephrologists who typically use anti-hypertensive medications as a first line of defense. Only very rarely do they give patients any advice about diet. When patients press for further options they are offered more medications and are told that if they are lucky, eventually they will be transplanted.
Those patients who venture outside of mainstream medicine in search of other options are confronted with confusing and often contradictory information, much of which is inappropriate to their situation. When there is a vacuum of sound medical advice, the internet often fills in the gaps. The patient at least feels they are doing something and not just passively waiting to go on dialysis. However, some good advice is usually mixed with a lot of bad advice. When cranberry juice and herbal diuretics don’t stop the progression of chronic kidney disease, the patient often feels they have run out of options.
Patients who turn to alternative practitioners for advice on treating kidney disease often have high expectations and end up disappointed. The gaps in knowledge of nephrology among holistic doctors becomes apparent, particularly with advanced kidney disease. Without a clear understanding of chronic kidney disease, unfortunately patients and practitioners alike often default to many of the prevailing myths surrounding kidney disease.
In this article we will look at some of the common misconceptions around kidney disease and how holistic physicians can better serve their renal patients.
Not using proper terminology
Kidney patients experience a huge gap between their experience with their nephrologist and their holistic practitioners. Not only do they operate from different paradigms, they don’t even seem to speak the same language. This leaves the patient confused but also contributes to a sense of mistrust from mainstream medicine. How can another practitioner address the kidney patient’s concerns if they misuse common terminology?
Kidney function refers to the kidney’s filtration ability and only this. The kidneys have many functions including regulating blood pressure, regulating the pH of the blood and producing erythropoietin, but the term kidney function refers only to the ability of the kidneys to filter out uremic wastes. A patient could have any type of kidney ailment from nephrotic syndrome to polycystic kidney disease to chronic kidney infections, and these conditions are serious, but if the kidney’s ability to filter wastes has not been compromised, they have 100% kidney function.
Kidney failure refers only to stage 5 chronic kidney disease. There is no such things as stage 3 or stage 4 kidney failure. There is chronic kidney disease which comes in stages, where the kidneys are gradually deteriorating and losing function. If chronic kidney disease continues to progress, it leads to kidney failure. Kidney failure is the state in which the kidneys have lost the ability to filter uremic wastes to the point where lifesaving measures are necessary. If creatinine is normal or just mildly elevated, the patient is not in kidney failure.
Patients in kidney failure may retain some residual function and produce some urine, but if the filtration rate is not high enough to sustain life, they are in renal failure. Residual function may include a high volume of urine, as the kidneys lose the ability to concentrate urine. But this urine is mostly water as the uremic compounds are not being filtered out and remain in the bloodstream.
Not understanding how calculations of kidney function work
The most common measurement of kidney function used is eGFR (estimated glomerular filtration rate). This is often taken as what percentage from out of 100% the kidneys are currently operating. It is also used to grade chronic kidney disease. Stage 5 is an eGFR under 15 and considered not enough activity in the kidney to sustain life. Intervention in the form of dialysis or a transplant will be necessary at this point.
However, one should consider how eGFR is calculated. Four values are plugged into a formula that includes creatinine, age, gender, and race. Creatinine is one uremic waste product that the kidneys need to clear. There are more than 3,000 different uremic waste products that the kidney handle, but creatinine tends to be the most stable.1 Creatinine is a waste product that comes from muscle tissue and since muscle mass does not shift significantly from one day to the next, creatinine tends to be more reliable than other potential markers. BUN (blood urea nitrogen) is also a uremic waste product, but BUN comes from dietary protein and can shift rapidly based on protein intake.
Age is also a factor in calculating eGFR. Some loss of kidney function is part of the aging process, and age-related kidney decline can lead to kidney failure in an otherwise healthy individual. However, it is important to know that anyone over age 60 will have a low eGFR no matter how healthy they are. This is simply how the formula is designed.2 Many elderly patients have consulted the author in a panic because their eGFR is low. It is important for practitioners to keep this in mind and look to the creatinine level directly to judge the patient’s situation.
Since men have a greater muscle mass than women, their creatinine will run higher. This is why gender is factored into the calculation for eGFR. Race is also factored in as those of African descent tend to have a higher baseline creatinine. However, many practitioners encounter the extremely fit young man who has a high creatinine and low eGFR. This is due to the increased muscle mass and may not be indicative of kidney weakness. For these people, it is good to run Cystatin C, an altogether different indicator of kidney function that is not affected by muscle mass.3
Misinterpreting wide fluctuations
With healthy kidneys, measuring function is often straightforward: the amount of the waste product creatinine present per volume unit of blood. A creatinine under 1.0 or under 1.3 is a healthy kidney, and whether the patient drank water the day before will have little impact on the creatinine. As the creatinine creeps up above 1.3 toward 2.0 and beyond, small changes in hydration can result in wide readings. Dehydration will cause the creatinine to be more concentrated. While a healthy kidney tightly regulates the water balance, advanced kidney disease often brings large shifts in the numbers. This is not necessarily reflective of an actual shift in the kidney filtration.
It is not always straightforward whether or not the patient is dehydrated and if dehydration is shifting the serum creatinine. Dehydration may be apparent from the specific gravity on the urinalysis or a pH that is more acidic than usual. A high hemoglobin/ hematocrit may also indicate dehydration, but since these numbers tend to be low with chronic kidney disease, it may be difficult to tell.4 It is also important to know if the patient has been warned against drinking too much water due to concerns over cardiac stress with fluid overload.
Underestimating the relationship between filtration and blood pressure
Hypertension is easy for many patients to ignore, but once the damage to the kidneys becomes apparent, patients want to get on track. Now they’re ready to get serious, take their blood pressure medications and do holistic interventions to keep their blood pressure down. But much to their dismay, their kidney function doesn’t get better, it actually gets worse. The patient may interpret this as a side effect of their medication and blame the toxicity of the drug. They stop the blood pressure medication and their kidney function gets better, so in their mind clearly the drugs were the problem. And since their listlessness and fatigue seems worse with an alpha blocker or beta blocker, who can blame them?
Convinced that blood pressure medications are the biggest issue, the patient may want to leave well enough alone and think that out-of-control blood pressure is really not all that bad. Or if they’re seeking out alternatives, they believe that If only the blood pressure were managed naturally instead of with medications, it would be different. But much to their dismay, natural agents like Rauwolfia, celery seed, hibiscus, and magnesium don’t seem to help the kidney function either.
This is often a difficult situation and it can be hard to convince these patients that blood pressure management is essential. As the kidneys filter the blood across a pressure gradient, the more internal tension there is in the kidney, the better it will filter the blood. It’s often useful for the patient to compare this to cleaning with a sponge. The tighter one squeezes a sponge, the better it cleans. When the kidneys are weak and not filtering the blood well, the blood pressure goes up. This helps the kidneys filter out the waste products. A healthy kidney does not need elevated blood pressure to sustain normal filtration. Correcting the blood pressure did not damage the kidneys, it simply revealed how much damage had already taken place. And like a sponge that is squeezed too vigorously and becomes worn out, the extra wear and tear of uncontrolled blood pressure will make the situation worse in the long term, even if it temporarily makes the serum creatinine better.5
Patients coming to alternative practitioners often hope to be able to discontinue their prescription medications. They need to understand that with weak kidneys there will be a need for intervention to manage blood pressure most likely from this point forward.5 At best they may be able to reduce the dosage or switch to some agent with fewer side effects. The worst course of action would be to abruptly stop blood pressure medication, especially since there is the possibility of rebound hypertension making the situation much worse.
It is important for the patient and the practitioner to anticipate that once out-of-control blood pressure is brought under control, there may be a sudden elevation in serum creatinine. Understanding the relationship between blood pressure and kidney filtration is necessary to understand the patient’s situation. Once the blood pressure is normalized, then evaluating the serum creatinine will give a better picture of the kidney’s filtration.
This is true not only for hypertension but also for hypotension and bradycardia. If an elderly patient exhibits low blood pressure and a slowed heart rate, do not jump to the conclusion that high creatinine means kidney dysfunction. There may simply be not enough pressure for filtration to take place. Normalize the blood pressure and heart rate first, and then see if the creatinine goes back down to an acceptable baseline.
Using diuretics to build kidney function
A diuretic is a stimulant. It temporarily pushes the kidney to expel more water and nothing more. It does not address the root cause of chronic kidney disease or protect the parenchymal tissue of the kidney from damage. One would not use a stimulant for other chronic conditions. One would not prescribe large doses of coffee for adrenal fatigue, and yet herbal diuretics are used as a panacea for all renal problems.
While anuria and oliguria are a problem in advanced kidney disease, as the kidneys break down and lose the ability to produce urine, herbal diuretics are not a solution. Like flogging a dying horse, demanding that it go faster, diuretics only serve to push an already weakened state. This is often difficult for the patient to accept as they believe that kidney cleanse products they purchased from the health food store are helping and they take the increased urine volume as evidence.
This is not to say that diuretics don’t have a place. When water retention is a serious issue, diuretics – either natural or by prescription – can provide relief. Diuretics can also be an important line of defense against persistent hypertension. Just don’t expect uva ursi, juniper, or parsley to help the kidneys filter wastes any better. The urine will be in a greater volume, but the kidneys are not any stronger.
Treating all kidney problems the same
It is amazing that so many natural kidney support formulas try to be all things to all people. Herbs for treating kidney stones, urinary tract infections, glomerulonephritis, and hypertension are often thrown together in one formula. While kidney stones may lead to chronic kidney disease, these conditions are not interchangeable. Some lay people are under the impression that renal lithiasis is rampant, and all people would benefit from a purification program to push these kidney stones out. This, however, is not the case with a prevalence of kidney stones in the United States at only 8.8% of the population.6
Formulas for kidney stones often contain an agent like Chanca piedra or Hydrangea arborescens to address the issue, as well as a demulcent like slippery elm and a diuretic. Formulas for urinary infections will typically have D-mannose, cranberry and also maybe a diuretic. Formulas to support kidney filtration may have cordyceps or rehmannia included. Hibiscus sabdariffa is an herb with multiple benefits as it may inhibit the formation of kidney stones,7 inhibit urinary tract infections,8 and support kidney function.9 But this is an exception. For most kidney patients, clarifying the problem is important for individualized treatment. A one-size-fits-all formula will have items they don’t need and probably won’t give an adequate dose of what they do need.
Expecting water to cleanse all
Clinical dehydration is certainly bad for the kidneys. Dehydration can also elevate creatinine on a blood draw, making kidney function appear worse than it really is. For many patients not drinking water is just a habit and their sense of thirst may be off. However, going to the opposite extreme brings its own problems.
This was one area where as a kidney patient, the author found agreement working with both a nephrologist and an OMD (Oriental Medical Doctor). The nephrologist was adamant that excess fluids would not help the kidneys get rid of more uremic waste. The same waste is passed but the urine is simply more dilute. The OMD for his part concurred. By the tenants of his practice, all things must be in balance including water.
It was the holistic doctors the author encountered who were of the mindset that if a little is good more must be better. For kidney patients in an early stage, an excess of water can cause an electrolyte disturbance. For patients with kidney failure, fluid overload can lead to congestive heart failure and shortness of breath.
For the holistically minded who have been told over and over that water is cleansing, the situation for those with kidney failure can be shocking. Fluid restrictions would seem counterintuitive when one is full of uremic toxins. However, producing urine is an active process on the part of the kidneys, and this production stops with kidney failure. The patient may be anuric with no urinary output or oliguric with very little output. The author has encountered holistic practitioners who questioned whether they should try to shift the urinary pH to a more acidic or alkaline balance in a patient with kidney failure. The fact that there is no urine and an entire bodily function has shut down did not immediately register.
Inferring too much from an urinalysis
The urinalysis should be a complement to the blood work to provide a more complete picture. Patients often read online that cancer thrives in an acidic body, and therefore they must alkalize their system. The author has encountered many patients who decide that since their urine has an acidic pH, their body is too acidic. They will then set up the goal of a neutral urinary pH to alkaline the body.
It is actually a healthy kidney that is able to expel metabolic acids. A weak kidney unable to filter out uremic wastes will pass mostly water, with a neutral pH. Also, certain bacteria and UTI may be associated with a high pH. In order to achieve a more alkaline urine, the patient usually needs to severely cut back on protein, a diet that will ultimately be unsustainable.
Going to extremes in diet
Protein increases the workload of the kidneys and a high protein diet will lead to higher levels of BUN. And when patients are afraid of kidney failure they’re willing to go to extremes to cut the protein out of their diet. They may cut protein out or even take up fasting to help their kidneys. But although this self-imposed marasmus or kwashiorkor will improve their BUN, it often comes at a price.
As the body strives for homeostasis, self-correcting mechanisms kick in. Blood albumin must be maintained; and without dietary protein, the body will take protein out of the muscles. Although protein deprivation may temporarily alleviate some kidney stress, the resulting sarcopenia will ultimately be to the patient’s detriment.10
Protein deprivation can bring a host of issues for many types of kidney patients. This is especially true with diabetic kidney issues. The patient is careful to avoid carbohydrates but doesn’t want to do too much protein either.11 Often the patient feels there are no acceptable options. For the pediatric patient, protein is necessary for growth; and for the kidney patient also fighting infections, protein is necessary for the immune system.
Slightly lower protein may be helpful, but moderation is key. In general, between 0.8 and 1.0 grams of protein per kg of body weight may work. For patients with very low filtration 0.6 grams of protein per kg of body weight may be used for a short time. This calculation may need to be adjusted if the patient has more adipose tissue. Greater body fat would not allow for greater protein consumption. In that case, calculations can be made using ideal weight for height and build rather than the actual weight.
Demonizing all dairy
Protein puts stress on the kidneys, but is dairy protein really worse than other types of protein? Kidney patients are often under the impression that all milk products are especially detrimental to kidney health, but is that really the case? Kefir has actually been shown to be helpful for diabetic nephropathy,12 and there is evidence that whey and casein decrease kidney inflammation and renal damage.13 While red meat, poultry, and seafood raise uric acid, dairy products will not. Some dairy products are more concentrated in phosphorus than others, but it is not the case that all dairy must be eliminated for every kidney patient.
Going to extremes cutting out minerals
When patients first learn that they have kidney trouble, the initial response is often to cut way down on sodium intake. Cutting out processed foods, canned soups, and preserved meats and eating in restaurants less often is a good first step. Drastically reducing sodium will also greatly improved edema. However, the body tightly regulates sodium in the blood and there will be diminishing returns if the patient goes to an extreme cutting out sodium. Blood pressure will only decrease a limited amount, as other factors besides sodium are driving the hypertension.14 Depending on the circumstances, foods naturally high in sodium like celery, tomato, or spinach may be beneficial. Whether the patient consumes 1,000 mg of sodium or 1,200 or 1,500 a day is usually not of great consequence. As long as the patient is not well over 2,000 mg of sodium, they do not need to be continually counting the mg of sodium in all of their food.
Kidney patients may also be mindful of potassium consumption. Unlike sodium, there are no hormonal regulators keeping potassium in homeostasis. Under normal circumstances a healthy kidney will expel potassium every time the patient urinates. Problems come with late stage kidney disease when the kidneys no longer pass potassium through the urine, potentially leading to a dangerous state of hyperkalemia. But this danger comes only from late stage kidney disease (or potentially from potassium sparing diuretics). The problem comes when the patient starts a low potassium diet prematurely. If the kidneys are still healthy enough to excrete potassium, there is no benefit to a low potassium diet. It does not reduce stress on the kidneys and cuts the patient off from many healthy fruits and vegetables.
Ignoring phosphorus
Phosphorus is a mineral that puts more stress on the kidneys, but one can only go so far in eliminating phosphorus from the diet. Some phosphorus in the diet is unavoidable as phosphorus naturally occurs with protein. That is unless the patient completely eliminates protein and takes amino acid supplements, a drastic measure that few patients are able to sustain for an extended period of time. Some dietary measures can minimize the patient’s phosphorus intake. Whole grains like quinoa and whole wheat are high in naturally occurring phosphorus. However, naturally occurring phosphorus is usually bound and not fully absorbed. Added phosphorus like phosphoric acid in soft drinks, however, are absorbed at virtually 100%. Many processed foods and fast foods also contain phosphate-based additives.15 This may even be present with food considered healthy like rice milk fortified with tricalcium phosphate.
Often unconsidered are sources of phosphorus from dietary supplements. Sometimes the presence of phosphorus is obvious from the name such as phosphatidylserine or phosphatidyl choline. It may also be added to the supplement as dicalcium phosphate. Krill oil, which is a phospholipid, is also a potential source of phosphorus. With late stage kidney disease, it is often necessary to take a phosphorus binder; but eliminating extra sources of phosphorus will make the situation easier to manage.
Processing natural vitamin D is normally handled by a healthy kidney, and many kidney patients have chronically low levels of vitamin D. But patients and holistic practitioners may be overzealous in correcting low vitamin D, as vitamin D increases the uptake of phosphorus. Some patients unable to manage their phosphorus do well to reduce their intake of vitamin D. If the nephrologist has prescribed calcitriol, additional vitamin D supplementation may be unnecessary. Continual monitoring of blood work will help clarify the patient’s needs. It is often good to have a target within normal range but on the lower side of normal.
Being afraid to use magnesium
Many people group electrolytes together and assume that since too much potassium is dangerous, magnesium is also dangerous. But high magnesium does not disrupt the heart the way high potassium does. At worst the patient might experience a loose bowel with too much magnesium.
There are multiple benefits of magnesium for the kidney patient and, like the population at large, magnesium levels may be low. Magnesium is a natural calcium channel blocker, and it also helps balance blood sugar. Even dialysis patients, who don’t eliminate magnesium in their urine, benefit from magnesium supplementation as it reduces calcification of the blood vessels.16
Expecting too much from diet alone
Diseases of the kidney such as IgA nephropathy, FSGS or polycystic kidneys are complex and multifactorial. In practice the author uses a combination of supplements, dietary strategies, and lifestyle changes (mild exercise, hydrotherapy and addressing sleep habits) to address chronic kidney disease. This is especially true with advanced kidney disease where decreased kidney filtration can impact a broad range of issues from cardiovascular health to bone density. Yet a surprising number of kidney patients want to address their issues with diet alone.
Many patients are under the impression that if only they can eliminate the offending food that’s triggering their inflammation, the kidney problem will resolve. This is usually perceived as getting to the root of the problem, but in practice after a long series of tests and elimination diets, not much shifts. The etiology of many renal conditions may involve a genetic predisposition but many times the condition is considered idiopathic, probably involving a variety of factors. And while many patients are busy sorting out the fine details of their diet, their kidneys are continuing to break down.
Unrealistic expectations of the kidney’s capacity to heal
Patients looking to alternative medicine sometimes believe that the body has an unlimited ability to regenerate. While some tissues of the body do have a great regenerative potential, the kidneys are not one of them. TCM acknowledges this as a weakening of the Jing with advancing years. Even without kidney disease, our nephrons are breaking down with the passing years, starting in our twenties.
Young children may outgrow conditions such as minimal change nephrotic syndrome. The kidneys are generally proportionate in size to one’s fist, and as children grow their kidneys grow. New kidney cells are still forming as there is active mitosis in a growing kidney. Once the individual is full grown, there is a limited capacity for the kidneys to regenerate. For adult kidney disease, we are maintaining the kidneys and preventing further decline.
Aggressive liver detox
The liver and the kidneys are both organs of elimination, and there are some conditions that effect both such as heptorenal syndrome and cystic kidneys that also involve liver cysts. Many traditional liver herbs are also beneficial to the kidneys. Silymarin can protect the kidneys from toxicity,17 and curcumin can support kidney filtration.18 Berberine can also help the liver and protect the kidneys.19 However, sometime patients and practitioners have unrealistic expectations of healing the kidney by correcting the liver. Aggressive liver detoxification will not be helpful if it pushes too much too fast.
Heavy metals, environmental toxins, and occupational exposure can tax the body’s detox systems; but if the kidneys are struggling to eliminate basic metabolic wastes like creatinine and BUN, it is important not to push too hard. The liver processes toxins through phase I and phase II detoxification and after these lipid soluble toxins become water soluble, they are handled by the kidneys. Often kidney patients are eager to detoxify, and they find that mainstream nephrology doesn’t even acknowledge their concerns. However, liver detox should be a gradual process for kidney patients.
Aggressive use of colonics
When a major organ of elimination is taxed, it makes sense to support the body’s other channels of elimination. Constipation is certainly a problem to be avoided, but aggressive use of colonics may be more fluid than the patient can handle. It could also make it difficult to manage electrolytes with a dramatic sudden shift. Some patients are given prescription laxatives like Kionex to help the body eliminate potassium. Patients could also use a distilled water enema to lower potassium, but the volume of fluid with a colonic can be problematic.
Avoiding dialysis at all costs
Traditional Chinese medicine states that fear is detrimental to the kidneys; and for most patients, there are few things more fear-provoking than the thought of dialysis. Like most fears looming large in one’s mind, the thought is often worse than the reality. The author writes this having experienced fourteen years of hemodialysis.
Avoiding dialysis can be a good motivation for change, and natural therapies can be an important part of slowing the progression of chronic kidney disease. But when the kidney filtration is not strong enough to sustain life, it’s time to be realistic about the patient’s options. Some patients fear the machine more than the damage of kidney failure itself and need to understand that they will be better off having toxins mechanically removed from the body. The author has seen patients with creatinine as high as 18, holding out for a transplant, unwilling to face the dialysis machine. These patients need to understand just how dangerous it is to avoid dialysis at any cost.
Working with a TCM practitioner, the author was urged to watch comedy on a regular basis. Fear is the body’s fight or flight responses, while laughter is the opposite state, breaking up the internal tension of fear and giving the body the message, ‘danger averted’. Interestingly, a study on survival rates for dialysis patients found scoring high on sense of humor in self-assessment was a huge predictor of long term survival.20 Holistic practitioners may have their own strong feelings against dialysis, but it will ultimately be for the patient’s best interest to maintain a positive attitude.
A holistic approach to kidney disease can dramatically improve a patient’s overall health and well-being, but patients and practitioners alike often hold notions that are at odds with the reality of their situation. With a balanced approach, it’s possible to address the concerns of chronic kidney disease and avoid the common pitfalls. A better understanding of nephrology will allow natural medicine to offer more targeted therapies.
References
1. Urine Metabolome website. The Metabolomic Innovation Centre. Available at: http://www.urinemetabolome.ca. Accessed March 18, 2018.
2. Raman M, et al. Estimating renal function in old people: an in-depth review. Int Urol Neprol. 2017 Nov;49(11):1979-1988.
3. Baxmann A, et al. Influence of Muscle Mass and Physical Activity on Serum and Urinary Creatinine and Serum Cystatin C. Clin J Am Soc Nephrol. 2008 Mar; 3(2): 348–354.
4. Holsworth R, Cho Y, Weidman J. Effect of hydration on whole blood viscosity in firefighters. Altern Ther Health Med. 2013 Jul-Aug;19(4):44-9.
5. Tsai W, et al. Association of Intensive Blood Pressure Control and Kidney Disease Progression in Nondiabetic Patients With Chronic Kidney Disease: A Systematic Review and Meta-analysis. JAMA Intern Med. 2017 Jun 1;177(6):792-799.
6. Scales C, et al. Prevalence of Kidney Stones in the United States. Eur Urol. 2012 Sep;62(3).
7. Laikangbam R, Damayanti D. Inhibition of calcium oxalate crystal deposition on kidneys of urolithiatic rats by Hibiscus sabdariffa L. extract. Urol Res. 2012 Jun;40(3):211-8.
8. Chou S, et al. Exploring the effect and mechanism of Hibiscus sabdariffa on urinary tract infection and experimental renal inflammation. J Ethnopharmacol. 2016 Dec 24;194:617-625.
9. Seujange Y, et al. Hibiscus sabdariffa Linnaeus aqueous extracts attenuate the progression of renal injury in 5/6 nephrectomy rats. Ren Fail. 2013;35(1):118-25.
10. Pereira R, et al. Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transplant. 2015 Oct;30(10):1718-25.
11. Campbell A, Rains T. Dietary protein is important in the practical management of prediabetes and type 2 diabetes. J Nutr. 2015 Jan;145(1):164S-169S.
12. Punaro G, et al. Kefir administration reduced progression renal injury in STZ-diabetic rats by lowering oxidative stress. Nitric Oxide. 2014 Feb 15;37:53-60.
13. Singh A, et al. Diets enriched in whey or casein improve energy balance and prevent morbidity and renal damage in salt-loaded and high-fat-fed spontaneously hypertensive stroke-prone rats. J Nutr Biochem. 2016 Nov;37:47-59.
14. He F, Li J, Macgregor G. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013 Apr 3;346:f1325.
15. Cupisti A, Kalantar-Zadeh K. Management of natural and added dietary phosphorus burden in kidney disease. Semin Nephrol. 2013 Mar;33(2):180-90.
16. Tzanakis I, et al. Magnesium retards the progress of the arterial calcifications in hemodialysis patients: a pilot study. Int Urol Nephrol. 2014 Nov;46(11):2199-205.
17. Bin F, et al. Silymarin protects against renal injury through normalization of lipid metabolism and mitochondrial biogenesis in high fat-fed mice. Free Radic Biol Med. 2017 Sep;110:240-249.
18. Ghosh S, et al. Curcumin ameliorates renal failure in 5/6 nephrectomized rates: role of inflammation. Am J Physiol Renal Physiol. 2009 May;296(5):F1146-57.
19. Li H, et al. [Effects and mechanisms of berberine on the hypertensive renal injury rats induced by enriched high fat-salt-fructose diet]. Zhong Yao Cai. 2011 Mar;34(3):412-5.
20. Svebak S, Kristoffersen B, Aasarod K. Sense of humor and survival among a county cohort of patients with end-stage renal failure: a two-year prospective study. Int J Psychiatry Med. 2006;36(3):269-81.
Myth Busting Common Misconceptions of Kidney Disease was originally published in Townsend Letter, #419, June 2018. Used with permission. You are invited to subscribe to the Townsend Letter.


