Lecture by Dr. Koren Barrett, N.D.
Attendee: Joanne Quinn, PhD, RMA
adrenalsystem.jpg
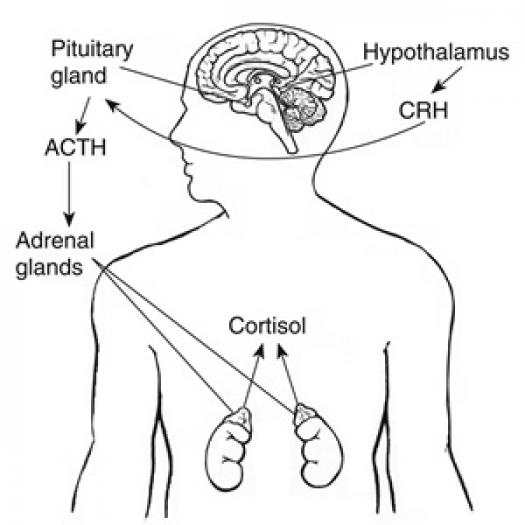
Illustration from National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
The hypothalamus sends CRH to the pituitary, which responds by secreting ACTH. ACTH then causes the adrenals to release cortisol into the bloodstream.
The adrenals are a part of the hypothalamus / pituitary / adrenal axis (HPA axis). There is a complicated communication system that creates cross talk via neurotransmitters and hormones.
Typically when a person is experiencing fatigue and sleep issues the practitioner will first look for thyroid dysfunction. If this is not the case then the next place to look are the adrenals.
The adrenals are small organs that sit on top of each kidney and produce among other things, cortisol and DHEA. Within the HPA axis the communication is in a loop. The hypothalamus releases corticotrophin releasing hormone (CRH) which stimulates the pituitary to release ACTH. This in turn stimulates the adrenals to release cortisol. As the level of cortisol gets too high it sends a message to the hypothalamus to quit releasing CRH. The adrenals typically release cortisol in a cyclic fashion known as pulsatile.
Cortisol, in a balanced individual, should be highest in the morning, waking you up. Then the levels decrease throughout the day being lowest at night to allow sleep. Cortisol is an important hormone, known as the "stress hormone." It regulates the metabolism of carbohydrates, fats and proteins. It is the hormone that saves us in the event of an acute stress coining the term "fight or flight." It is meant to give the body the reserves of strength it needs in these instances and then the body returns to homeostasis once the crisis is over. However, in our lifestyles of chronic stress our bodies continually release cortisol due to environmental, psychosocial, physiological and biological stresses. When cortisol levels remain high there are destructive side effects including conditions of low progesterone because the adrenals convert progesterone to cortisol. Bone and muscle mass are diminished. Systems for healing, metabolism and immunity are depressed and blood pressure is raised. The appetite is stimulated causing weight gain, especially in the abdomen. One function of cortisol is to release glucose into the blood system when blood sugar gets too low. When cortisol is too high, unnecessary glucose is released and cannot be burned up, ultimately being stored as fat. Finally, individuals experience mood alterations and insomnia.
DHEA is another hormone released by the adrenals. Like progesterone, it can be converted into cortisol. This hormone helps in the creation of muscle mass and bone density. DHEA and cortisol do a dance together that helps the practitioner determine the state of health of the adrenals. Under normal stress conditions, both cortisol and DHEA are increased but return to normal after the stress is gone. Under prolonged stress DHEA will remain within normal ranges, but the cortisol will be increased. The next phase is known as decompensation where the DHEA will be low and the cortisol will vacillate but generally be high. In this condition people feel wired yet tired. The final stage is adrenal fatigue/exhaustion. DHEA will be low as will be cortisol.
Various other systems are affected by an imbalance of cortisol. As mentioned above it can cause weight gain. Women experiencing perimenopause and menopause can be affected. With the body producing less estrogen, the adrenals take over estrogen production through the conversion of other hormones. If these hormones are needed to produce cortisol, then other hormone levels suffer. Cortisol also inhibits the function of serotonin. This is also a complicated communication loop, with serontonin depressing the production of melatonin and ultimately causing insomnia. In the case of hypoglycemia (low blood sugar), cortisol is released to increase the glucose in the blood. This false sense of starving suppresses the thyroid (another metabolizing organ), lowering metabolism for up to 18 hours and ultimately results in weight gain. At night (generally at 3am) if the blood sugar gets too low, cortisol will be released and wakes the individual with a start and makes it nearly impossible to return to sleep. This is a common complaint. Sometimes eating protein prior to going to bed can help maintain adequate levels of blood sugar throughout the night.
By doing adrenal saliva testing the patient can see the pulsatile levels of free cortisol and DHEA during the 24 hours of the day to determine adrenal health. This test looks at cortisol and DHEA levels at 7am, 12noon, 3pm and 11pm.
If a person determines there is a cortisol imbalance there are many alternative and complementary treatments to return the adrenal to a healthy balance.
- Stress Management: get good sleep, exercise, seek psychotherapy and relax.
- Treat for hypoglycemia: eat 5 times a day, eat organic whole foods, eat protein, fat and complex carbohydrates at every meal.
- Remove stimulants: avoid caffeine, treat for food allergies, avoid fasting and detoxing.
- Cholesterol: keep them at a high enough level since they are the precursor for the production of all hormones, be careful with the use of statin drugs as they can lower cholesterol to dangerous levels, eat food including animal protein, butter, coconut oil and coconut milk, however in moderation.
- DHEA supplementation: follow the guidance of your practitioner.
- Glandular supplements for low cortisol: animal adrenal cortex, licorice (but not with high blood pressure), ashwagandha, Siberian ginseng, panax ginseng rhodiola and tongkat ali.
- Other nutrients: Vitamin C, B5 and Zinc.
The bottom line is that it is very easy to test for adrenal dysfunction and there are very effective approaches to return the adrenals to balance. There are many companies who have developed nutritional supplements to support all stages of adrenal stress.



