ifm21centurymedicinepaper.jpg
IFM's white paper, 21st Century Medicine: A New Model for Medical Education and Practice
Executive summary
By David S. Jones, MD; Laurie Hofmann, MPH; Sheila Quinn
In early 2009, an extraordinary degree of public attention was focused on healthcare reform. In Washington, DC, two hearings were held before the Senate Committee on Health, Education, Labor and Pensions, and the Institute of Medicine of the National Academy of Sciences hosted a Summit on Integrative Medicine and the Health of the Public. In New York City, a major conference on Integrative Health Care was held. The January/February 2009 issue of Health Affairs was devoted entirely to The Crisis in Chronic Disease. Why?
We know with certainty now that rapidly rising rates of complex, chronic disease are creating an unsustainable burden on the national economy in both direct (e.g., treatment) and indirect (e.g., lost productivity) costs. The $1.3 trillion estimated to be the cost of chronic disease today may well grow to $4.2 trillion within 15 years. Health professionals struggle every day to cope with the increase in suffering and disability that accompanies this modern epidemic. At a time when many other urgent pressures on the national economy command our attention, we absolutely must sustain our focus on the system-wide changes in health care that will be required in the years ahead if the most severe consequences of this epidemic are to be avoided.
A careful examination of the evidence on both performance and costs in American health care convincingly demonstrates the urgent need for this transformation. We have been taught to believe that we have the best health care in the world, but the facts do not support such an assessment. We spend about twice as much per capita as other industrialized countries and yet we rank shockingly low on most parameters of health.
Many diverse influences are responsible for the current state of the public's health (see Figure 1). It is not enough, however, to demonstrate, as many experts have done, that the majority of today's chronic diseases could be prevented or ameliorated by changes in lifestyle, and then suggest that patient responsibility and self-care can take care of the problem. We must also ask what contributes to such unhealthy lifestyles and how can we best equip clinicians to serve the patients who are living every day under those pressures. It is critical that we understand how great a proportion of environment and lifestyle is influenced by conditions beyond the control of individual patients — not only the genetic vulnerability one is born with, but increases in environmental toxicity, the homogenization and denaturing of the food supply, the influence of sedentary technology on jobs, education, and entertainment, the powerlessness and despair of poverty, the debility produced by chronic stress, and the fragmentation of family and community life that leads to isolation and a lessened sense of purpose and meaning. These are all complex problems that took many decades to create and that will require a long-term national effort and effective leadership in public policy to alter. We recognize — and emphasize — that not only must we change healthcare and medical education (the primary focus of this paper), but over the next decades we must also change the practices and priorities of our political, social, and economic structures to achieve fundamental change in the public's health.
ifmfig1.jpg
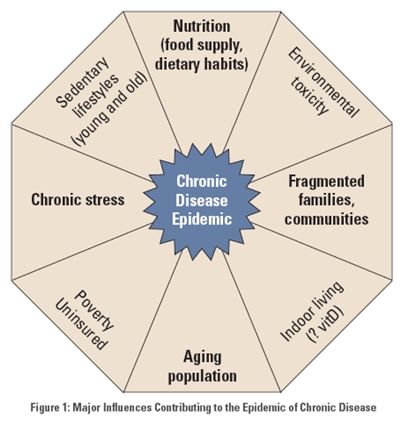
Image provided by The Institute for Functional Medicine
Figure 1: Major influences contributing to the epidemic of chronic disease
In order to change our future, however, we must thoroughly understand our past. Therefore, after presenting an overview of the paper (Chapter 1), we focus first on exploring the dominant influences that have helped to shape the current crisis in health care (Chapter 2). Next, we present and discuss the most prominent models that have been proposed for the future (Chapter 3). The implications of these issues for the practicing clinician are then analyzed (Chapter 4). And last, a preferred model for 21st century medicine is presented (Chapter 5). It is important to recognize that even if patients do everything it is possible for individuals to do for their own health (an idealized state that is highly unlikely to be realized), we still have tens of millions of people with multiple chronic diseases, and well over 100 million with at least one,14 and both figures are on the upswing. All of these people need more effective therapeutic services, and everyone needs more effective disease prevention and wellness promotion strategies in order to cope with the pervasive environmental influences that make achieving health such a challenge.
The transformation of 21st century medicine from the prevailing acute-care model to a far more effective chronic-disease model will succeed only if we attack the underlying drivers of the epidemic — the complex, lifelong interactions among lifestyle, environment, and genetics — and if we engage the entire healthcare system in a concerted effort to implement a unified, flexible approach that can readily adapt to shifting needs and emerging evidence. The central purpose of this paper is to demonstrate that such changes are urgently needed and achievable.
In order to accomplish such an ambitious goal, several key objectives must be achieved. As discussed in the succeeding pages, these include:
- A shared understanding of the powerful, primary influence of lifestyle and environment upon genetic vulnerability in the initiation and progression of chronic disease must be matched with a therapeutic tool kit that reverses the trajectory toward disease and disability, promotes health, and empowers patients as full partners in the lifelong pursuit of wellness.
- A more balanced perspective on the appropriate uses of both evidence and insight must be integrated with broad-based clinical skills to establish the foundation for healing partnerships between practitioners and patients.
- A common set of principles, concepts, and practices that can be used by all health professionals must be taught and applied in clinical practice so that well-trained integrated healthcare teams can be deployed appropriately.
- A model that incorporates all these elements must pervade education, clinical practice, and research in both private and public arenas.
In this paper, we propose that functional medicine exemplifies the systems-oriented, personalized medicine that is needed to transform clinical practice, education, and research. The functional medicine model of comprehensive care and primary prevention for complex, chronic illnesses is grounded in both science (the Functional Medicine Matrix Model™; evidence about common underlying mechanisms and pathways of disease; evidence about effective approaches to the environmental and lifestyle sources of disease) and art (the healing partnership and the search for insight in the therapeutic encounter). Many years of developing, writing about, and teaching this model to thousands of clinicians in both private practice and academic medicine have demonstrated that functional medicine can enable us to reshape health care for the demands of the 21st century. Using this approach, a healing partnership between doctor and patient can flourish, new and useful insights can be achieved, and a broad array of assessment and therapeutic tools can be utilized by integrated healthcare teams.
About the Institute for Functional Medicine
The Institute for Functional Medicine (IFM) is a nonprofit, tax-exempt 501(c)3 educational organization that educates physicians and other healthcare practitioners in improving the assessment and management of complex, chronic disease through the use of functional medicine. The Institute's mission is threefold: to develop the functional medicine knowledge base as a bridge between research (both emerging and established) and clinical practice; to educate physicians and other healthcare providers in the basic science and clinical applications of functional medicine; and to communicate with policy makers, practitioners, educators, researchers, and the public to disseminate the functional medicine knowledge base more widely. IFM has developed a model of comprehensive care and primary prevention for complex, chronic illness that is grounded in both the science (the Functional Medicine Matrix Model™) and the art (the healing partnership in the therapeutic encounter) of clinical medicine that is now being implemented by functional medicine practitioners around the world.
The Institute for Functional Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. IFM offers educational publications and programs designed to raise the bar on clinicians' standard of care. Programs such as IFM's Functional Medicine Certification Program and Applying Functional Medicine in Clinical Practice (AFMCP) provide comprehensive clinical training for the assessment, treatment, prevention, and management of patients with complex, chronic disease. Other programs include IFM's Advanced Practice Modules, online Webinars, and the annual International Symposia on functional medicine. The Institute publishes textbooks, monographs, and other educational materials available for CME credits and offers clinicians a Forum for the shared exploration of emerging research and clinical applications to improve patient care and outcomes. Detailed information about the Institute, its educational activities, and membership can be found at The Institute for Functional Medicine.
Author David S. Jones, MD is the President of The Institute for Functional Medicine. He has practiced as a family physician with emphasis in functional and integrative medicine for over 25 years. He is a recognized expert in the areas of nutrition, lifestyle changes for optimal health, and managed care, as well as the daily professional functions consistent with the modern specialty of Family Practice. He is the Editor-in-Chief of the Textbook of Functional Medicine. Laurie Hofmann, MPH, is IFM's Executive Director and an advisor and consultant to several public healthcare and health education initiatives across the country. Sheila Quinn is consulting author and editor of 21st Century Medicine: A New Model for Medical Education and Practice and many other IFM publications including the Textbook of Functional Medicine.
For information on obtaining additional copies of 21st Century Medicine or to join us in IFM's vision and mission as a functional medicine practitioner, member, advocate, or sponsor, we invite you to visit The Institute for Functional Medicine website, call us at 800-228-0622, or write us at client_services@fxmed.com. To contact the authors of 21st Century Medicine or to submit comments or questions on this publication, please write to David S. Jones, MD at DavidJones@fxmed.com.
© IFM; reprinted with permission.


